Antibiotic Selection Tool
Find the Best Antibiotic for Your Situation
Answer a few questions about your infection and allergies to get a personalized recommendation among Duricef (cefadroxil) and common alternatives.
Select Your Infection Type
Allergy Information
When you’re prescribed an oral antibiotic for a skin infection, urinary tract infection, or respiratory issue, you’ll often hear the name Duricef. But how does it really stack up against other common antibiotics? This guide breaks down Duricef (cefadroxil) and the most frequently used alternatives, showing you the key differences in spectrum, dosing, side‑effects, and typical use cases so you can have a clearer conversation with your clinician.
Key Takeaways
- Duricef (cefadroxil) is a first‑generation cephalosporin with a broad gram‑positive coverage and modest gram‑negative activity.
- Cephalexin and cefuroxime are close relatives that differ mainly in dosing frequency and potency against certain bacteria.
- Amoxicillin and azithromycin belong to different drug classes, offering alternative pathways when a patient is allergic to beta‑lactams.
- Side‑effect profiles are generally mild, but gastrointestinal upset and allergic reactions are the most common across the board.
- Choosing the right antibiotic depends on infection type, patient allergies, dosing convenience, and local resistance patterns.
What Is Duricef (Cefadroxil)?
Duricef is the brand name for cefadroxil, a first‑generation cephalosporin antibiotic. It works by inhibiting bacterial cell‑wall synthesis, which leads to cell lysis and death. Approved in the UK and many other markets, Duricef is commonly prescribed for skin and soft‑tissue infections, uncomplicated urinary tract infections, and some respiratory infections caused by susceptible streptococci and staphylococci.
How Does Duricef Compare to Other Oral Antibiotics?
Below is a side‑by‑side look at seven widely used oral antibiotics. The table focuses on the attributes most relevant to patients: drug class, typical adult dosage, main infections treated, and notable pros or cons compared with Duricef.
| Antibiotic | Class | Typical Adult Dosage | Common Uses | Key Side Effects | Pros vs. Duricef |
|---|---|---|---|---|---|
| Cefadroxil (Duricef) | First‑gen cephalosporin | 500mg every 12h | Skin/soft‑tissue, uncomplicated UTI, streptococcal pharyngitis | Diarrhea, nausea, rash | Broad gram‑positive coverage; twice‑daily dosing is convenient |
| Cephalexin | First‑gen cephalosporin | 250‑500mg every 6h | Skin infections, ear infections (otitis media), uncomplicated UTI | Stomach upset, allergic rash | Similar spectrum but requires four times daily dosing for peak levels |
| Cefuroxime | Second‑gen cephalosporin | 250mg every 12h (axetil) or 500mg q8h (tablet) | Sinusitis, bronchitis, gonorrhea (off‑label), more resistant gram‑negatives | Diarrhea, metallic taste, dizziness | Better gram‑negative coverage; flexible dosing forms |
| Amoxicillin | Penicillin‑type beta‑lactam | 500mg every 8h | Otitis media, pneumonia, H.pylori eradication (with clarithromycin) | Rash, GI upset, rare liver enzyme elevation | Lower cost; excellent for many community‑acquired infections |
| Azithromycin | Macrolide | 500mg on day1, then 250mg daily for 4days | Chlamydia, atypical pneumonia, travelers’ diarrhea | Abdominal pain, QT prolongation, liver enzyme rise | Once‑daily dosing; good for patients with penicillin allergy |
| Penicillin V | Natural penicillin | 250‑500mg every 6h | Strep throat, rheumatic fever prophylaxis | Allergic skin reactions, GI upset | Very narrow spectrum; ideal when organism is known |
| Clindamycin | Lincosamide | 300mg every 6h | Skin and bone infections (MRSA coverage), anaerobic infections | Clostridioides difficile infection risk, metallic taste | Effective against certain resistant gram‑positives; not a beta‑lactam |
| Doxycycline | Tetracycline | 100mg twice daily | Lyme disease, acne, malaria prophylaxis | Sun sensitivity, esophageal irritation | Broad spectrum, long half‑life; can be used in patients allergic to beta‑lactams |
When Might a Doctor Choose Duricef Over the Others?
Duricef shines in situations where you need reliable gram‑positive coverage without the need for a twice‑daily schedule. Its pharmacokinetics allow steady blood levels with 12‑hour dosing, which can improve adherence compared with cephalexin’s four‑times‑daily regimen. If the infection is caused by susceptible streptococci or methicillin‑sensitive Staphylococcus aureus (MSSA), Duricef is often just as effective as amoxicillin but offers a broader safety margin against beta‑lactamase‑producing strains.
However, in regions with rising resistance to first‑generation cephalosporins, clinicians may prefer cefuroxime or a macrolide like azithromycin for respiratory infections that involve Haemophilus influenzae or atypical pathogens.
Safety and Side‑Effect Checklist
- Allergy risk: As a beta‑lactam, Duricef can trigger reactions in patients allergic to penicillins or other cephalosporins. Cross‑reactivity rates are around 5‑10%.
- GI upset: Nausea, vomiting, and mild diarrhea occur in roughly 10% of users. Taking the drug with food can lessen the discomfort.
- Kidney considerations: Dose adjustment may be needed for patients with severe renal impairment (CrCl<30mL/min).
- Rare events: Clostridioides difficile infection has been reported, though less frequently than with clindamycin.
Practical Tips for Patients
- Complete the full course even if you feel better; stopping early can promote resistance.
- If you miss a dose, take it as soon as you remember unless it’s almost time for the next dose-don’t double up.
- Store the tablets in a cool, dry place; no refrigeration needed.
- Report any rash, swelling, or breathing difficulty immediately-these could signal a serious allergic reaction.
- Hydrate well and consider a probiotic if you’ve experienced diarrhea on antibiotics before.
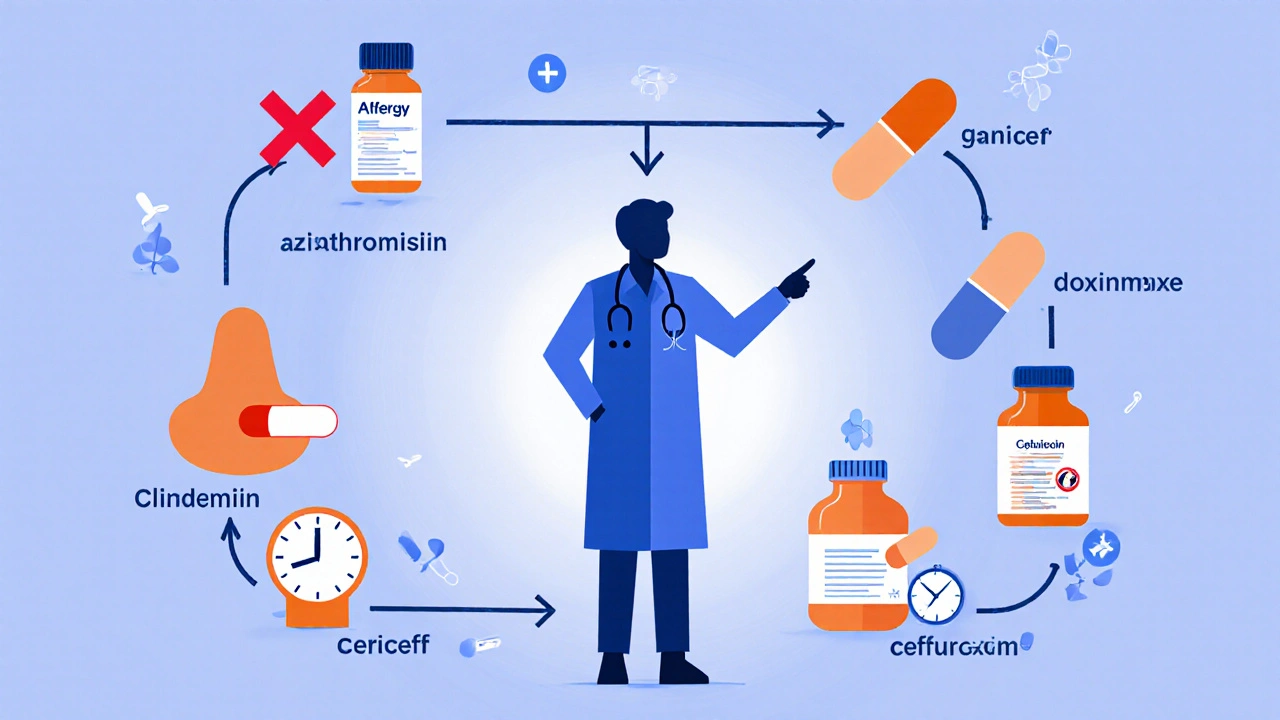
Decision‑Making Flowchart
Use the quick flow below to see whether Duricef or an alternative might be the best fit:
- Do you have a known beta‑lactam allergy? Yes → consider azithromycin, doxycycline, or clindamycin.
- Is the infection likely caused by MSSA or streptococci? Yes → Duricef or cephalexin are strong choices.
- Is the pathogen suspected to be a gram‑negative organism (e.g., H.influenzae)? Yes → cefuroxime or a macrolide may be better.
- Need for once‑daily dosing? Yes → azithromycin’s loading‑dose regimen could win.
- Cost sensitivity? Yes → amoxicillin and penicillin V are typically cheaper.
Frequently Asked Questions
Can I take Duricef with food?
Yes. While Duricef’s absorption isn’t dramatically affected by meals, taking it with food can reduce stomach upset, especially for sensitive individuals.
How long does it take for Duricef to start working?
Patients usually notice improvement within 48‑72hours, though the full course should be completed as prescribed to eradicate the infection completely.
Is Duricef safe during pregnancy?
Cefadroxil falls into pregnancy category B in the UK, meaning animal studies have not shown risk, but there are limited human studies. Your doctor will weigh the benefits against any potential risks.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one-don’t double up.
Can Duricef be used for severe infections?
For severe or hospital‑acquired infections, intravenous cephalosporins (e.g., ceftriaxone) are preferred. Duricef is best suited for uncomplicated community‑acquired issues.
Bottom Line
Duricef offers a solid balance of efficacy, dosing convenience, and safety for many common infections, but it’s not a one‑size‑fits‑all solution. Understanding the infection type, your allergy history, and local resistance trends will guide the best choice-whether that’s staying with Duricef, switching to a second‑generation cephalosporin like cefuroxime, or opting for a different class such as a macrolide or penicillin.
Always discuss your specific situation with a healthcare professional before starting or changing any antibiotic regimen.
