Immunosuppressant Pregnancy Risk Checker
Medication Safety Information
Pregnancy Risk
Select a medication to see pregnancy risk details
Fertility Impact
Select a medication to see fertility impact details
Action Steps
- Select a medication to see recommended action steps
- Select a medication to see recommended action steps
- Select a medication to see recommended action steps
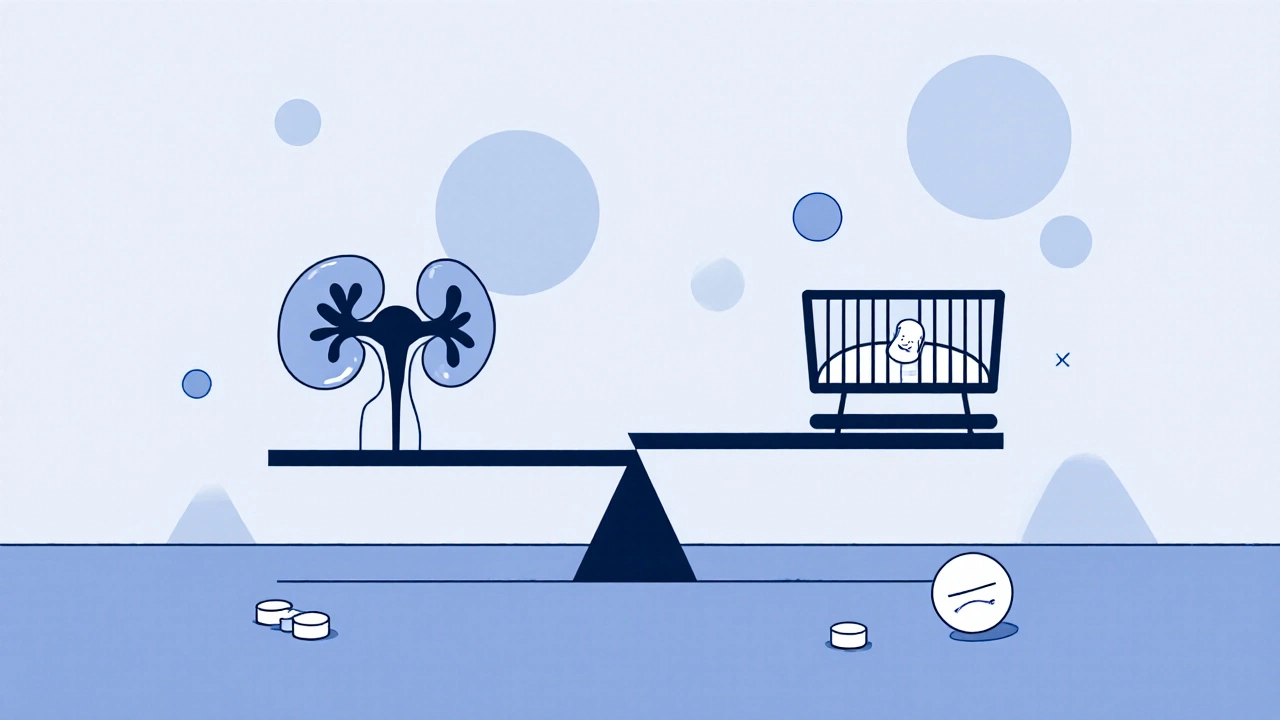
Planning a baby while on immunosuppressants isn’t just about timing-it’s about safety, science, and smart choices. Many people assume that if they’re managing a chronic condition like lupus, rheumatoid arthritis, or have had a kidney transplant, pregnancy is off the table. But that’s not true anymore. Thanks to better research and updated guidelines, immunosuppressants are no longer automatic barriers to having children. Still, the risks are real, and skipping the right prep can lead to serious consequences-for you, your baby, and your long-term health.
Not All Immunosuppressants Are Created Equal
If you’re taking one of these drugs, your next step isn’t to panic-it’s to find out which one you’re on and what it actually does to fertility and pregnancy. The difference between drugs is huge.Azathioprine is one of the safest. Over 1,200 pregnancies in studies going back to 2000 showed no increase in birth defects or miscarriages. It’s often the go-to choice for people planning to conceive. If you’re on this one, your doctor may just keep you on it, with regular blood tests to make sure your levels stay stable.
But others? Big red flags. Cyclophosphamide can permanently damage ovaries. For women, taking more than 7 grams per square meter of body surface area leads to permanent infertility in 60-70% of cases. For men, it can wipe out sperm production entirely in 40% of users-and that damage doesn’t always come back. This isn’t a drug you want to be on if you’re thinking about kids down the line.
Methotrexate is another no-go during pregnancy. It’s toxic to embryos. Even if you’re not trying to get pregnant, you need to stop it at least three months before you start trying. That’s not a suggestion-it’s a medical requirement. Same goes for chlorambucil, which is linked to kidney, heart, and urinary tract defects in babies. The FDA classifies it as a Category D drug, meaning there’s clear evidence of harm.
Then there’s sirolimus. Seven reported pregnancies involving this drug included three miscarriages and one baby born with major structural abnormalities. It’s still officially contraindicated in pregnancy. Belatacept, a newer drug, has only three documented cases of pregnancy so far-all ended in healthy babies. But that’s not enough data to call it safe. It’s promising, but still experimental in this context.
Steroids and Hormones: The Hidden Impact
Prednisone and other corticosteroids are often thought of as harmless in pregnancy. They’re used all the time for asthma, allergies, and autoimmune flares. But they’re not risk-free.These drugs interfere with the body’s natural hormone signals. In women, that can mean irregular ovulation or even stopped cycles. In men, it can lower testosterone and reduce sperm production. And it’s not just about getting pregnant-it’s about staying pregnant. Studies show steroid use increases the risk of premature rupture of membranes by 15-20%. That means your water breaks too early, which can trigger preterm labor.
That’s why doctors don’t just tell you to stop steroids before pregnancy. They tell you to lower the dose as much as possible, and only use it when absolutely necessary. If you’re on high doses (over 20 mg daily), your team may start tapering you down six months before you plan to conceive.
Male Fertility: The Overlooked Side
Most people think fertility is a woman’s issue. But when it comes to immunosuppressants, men are just as affected-and way less talked about.Sulfasalazine, commonly used for Crohn’s disease and ulcerative colitis, cuts sperm count by 50-60%. The good news? It’s reversible. Once you stop the drug, sperm numbers bounce back in about three months. But you need to plan ahead. Don’t wait until you’re trying to conceive to find out your count is low.
The FDA recommends semen analysis at three key points: right before starting the drug, after one full sperm cycle (about 74 days), and again 13 weeks after stopping. That’s not just bureaucracy-it’s how you know if your fertility is at risk.
And here’s the kicker: most of these drugs were approved decades ago, before regulators required testing for male reproductive side effects. So we’re still playing catch-up. Many men don’t even know their meds could affect their ability to have kids-until it’s too late.
When to Talk to Your Doctor-And What to Ask
If you’re on any immunosuppressant and thinking about having a baby, you need to start this conversation at least six months before you plan to conceive. That’s not a suggestion. That’s the minimum.Here’s what you need to ask:
- Is my current medication safe for pregnancy? If not, what’s the alternative?
- How long do I need to stop or switch before trying?
- Do I need fertility testing? For me? For my partner?
- Are there any fertility preservation options if my drug is high-risk (like cyclophosphamide)?
- What happens if my disease flares up during pregnancy?
Don’t wait for your rheumatologist or transplant team to bring it up. Bring it yourself. Most doctors assume you’re not thinking about kids-or they assume you already know. You don’t. And that’s okay. But now you do.
What Happens After You Get Pregnant?
Getting pregnant is just the first step. The real work begins after.For transplant patients, the biggest fear isn’t the baby-it’s organ rejection. Stopping or lowering immunosuppressants can trigger a flare-up that kills the transplant. That’s why your care team needs to be in sync: your nephrologist, your OB-GYN, your rheumatologist, and your fertility specialist.
Monthly blood tests for creatinine levels are standard. If your creatinine is above 13 mg/L before pregnancy, your risk of pre-eclampsia jumps. That’s a dangerous condition that can threaten both your life and your baby’s.
And your baby? Their immune system might be quieter than normal. Studies show newborns of mothers on immunosuppressants have significantly lower B-cell and T-cell counts. That means they’re more vulnerable to infections in the first year. Your pediatrician needs to know about your meds so they can watch for early signs of illness.

What About Breastfeeding?
Some drugs are safe. Others aren’t. And it’s not always obvious.Azathioprine is considered low-risk during breastfeeding. Only tiny amounts pass into breast milk, and studies haven’t shown harm to babies. Many moms continue on it.
Chlorambucil? Absolutely not. It’s known to enter breast milk and can damage a baby’s developing cells. You’re told to stop breastfeeding if you’re on it.
There’s no blanket rule. You need to check each drug individually. Ask your pharmacist to look up the LactMed database-it’s the gold standard for drug safety during breastfeeding.
What’s New? What’s Still Unknown?
The field has changed a lot since 2000. Back then, doctors had almost no data on children born to parents on these drugs. Now, most transplant centers have formal pregnancy protocols. That’s progress.But gaps remain. Belatacept looks good-but only three pregnancies have been recorded. Sirolimus is still banned, even though animal studies show no birth defects. Why? Because human data is too scary to ignore.
And what about long-term outcomes? Do kids exposed to immunosuppressants in the womb have higher rates of learning delays? Autoimmune issues later in life? We don’t know. No large, long-term studies have been done.
That’s why registries are being set up. If you’ve taken these drugs and had a child, your story matters. Ask your doctor if your hospital or clinic is tracking outcomes. Consider joining a registry. Your data could help the next person.
Your Next Steps
1. Write down every medication you’re taking-including supplements and over-the-counter drugs. 2. Call your specialist and say: “I’m thinking about having a baby. Can we review my meds?” 3. Ask for a referral to a reproductive endocrinologist or fertility specialist who’s worked with autoimmune or transplant patients. 4. Get tested-semen analysis for men, ovarian reserve testing for women. 5. Plan a timeline. Give yourself at least six months to switch meds, stabilize your condition, and optimize your health. 6. Don’t stop meds on your own. Stopping suddenly can cause organ rejection or a dangerous flare-up.Having a baby while on immunosuppressants isn’t easy. But it’s possible. And with the right planning, it can be safe. You’re not alone. Thousands of people have done this. You just need the right team-and the right information.
Can I get pregnant while taking azathioprine?
Yes. Azathioprine is one of the safest immunosuppressants for pregnancy. Studies involving over 1,200 pregnancies show no increased risk of birth defects or miscarriage. Most doctors continue it throughout pregnancy, especially for transplant patients or those with severe autoimmune disease. Regular blood tests are needed to monitor your levels and ensure your disease stays under control.
How long before trying to conceive should I stop methotrexate?
You must stop methotrexate at least three months before trying to conceive. It’s highly toxic to developing embryos and can cause severe birth defects. Even small amounts lingering in your system can be dangerous. Your doctor may recommend a blood test to confirm the drug is fully cleared before you start trying.
Do immunosuppressants cause permanent infertility?
Some do, some don’t. Cyclophosphamide can cause permanent ovarian failure in women and irreversible azoospermia in men, especially at higher cumulative doses. Sulfasalazine causes temporary low sperm count, which reverses within three months of stopping. If you’re prescribed a high-risk drug like cyclophosphamide, ask about fertility preservation-egg or sperm freezing-before you start treatment.
Is it safe to breastfeed while on immunosuppressants?
It depends on the drug. Azathioprine is considered safe, with minimal transfer to breast milk. Prednisone is generally safe at low to moderate doses. But chlorambucil, mycophenolate, and cyclophosphamide are not safe-these drugs can pass into milk and harm the baby. Always check with your pharmacist or doctor using the LactMed database before breastfeeding.
What are the risks to the baby if I’m on immunosuppressants during pregnancy?
Risks vary by drug. Some, like azathioprine, show no increased risk. Others, like sirolimus or chlorambucil, are linked to miscarriage and birth defects. Even safe drugs can affect the baby’s immune system-newborns may have lower white blood cell counts and be more prone to infections in their first year. Close monitoring by your pediatrician is essential.
Can men on immunosuppressants father healthy children?
Yes, but it depends on the drug. Sulfasalazine reduces sperm count but doesn’t harm sperm DNA-fertility returns after stopping. Cyclophosphamide can cause permanent infertility and may damage sperm DNA, increasing miscarriage risk. Men should have a semen analysis before starting treatment, and again 74 days after starting and 13 weeks after stopping. Avoid conception during active treatment with high-risk drugs.
Why is preconception counseling so important?
Because switching meds takes time, and your disease needs to be stable before pregnancy. Stopping a drug too soon can trigger a flare that harms both you and your baby. Starting a new drug too late can mean you’re still on something risky when you conceive. Preconception counseling gives you six months to make safe, informed changes-without rushing or guessing.