When your life changes-whether you’re moving cities, starting a new job, going through a breakup, or caring for a sick relative-your medication routine often falls apart. Not because you’re lazy or forgetful, but because your whole world has shifted. You’re exhausted. Your schedule is gone. Your support system is disrupted. And suddenly, that pill you took every morning at 8 a.m. doesn’t fit anymore. Medication adherence doesn’t just drop during these times-it crashes. Research shows that up to 70% of people miss doses during major life changes, and adherence can fall by over 30% within the first two weeks. This isn’t just about forgetting pills. It’s about losing control when you need it most.
Why Your Routine Breaks Down During Transitions
It’s not that you suddenly stopped caring. It’s that your brain is overwhelmed. When something big happens-like relocating or losing a job-your prefrontal cortex, the part responsible for planning and self-control, gets buried under stress hormones. Your body is in survival mode. Taking a pill at the same time every day? That’s a luxury your brain can’t afford right now. Studies from the Journal of Personality and Social Psychology show that people who feel they have no control over their situation are far more likely to abandon health routines. That’s why simply setting phone alarms or using a pill organizer often fails during transitions. Those tools assume your life is stable. It’s not. And trying to force your old routine onto a new reality just adds more stress. Real-world examples tell the same story. On Reddit’s r/ChronicIllness, 78% of users reported stopping their meds during a major life shift. The top triggers? Relocation (63%), job changes (58%), and relationship breakdowns (49%). One user wrote: “After my divorce, I stopped all my meds for three months. No one asked if my routine still worked. I just assumed I was supposed to figure it out alone.”The Three Lists: Reclaiming Control
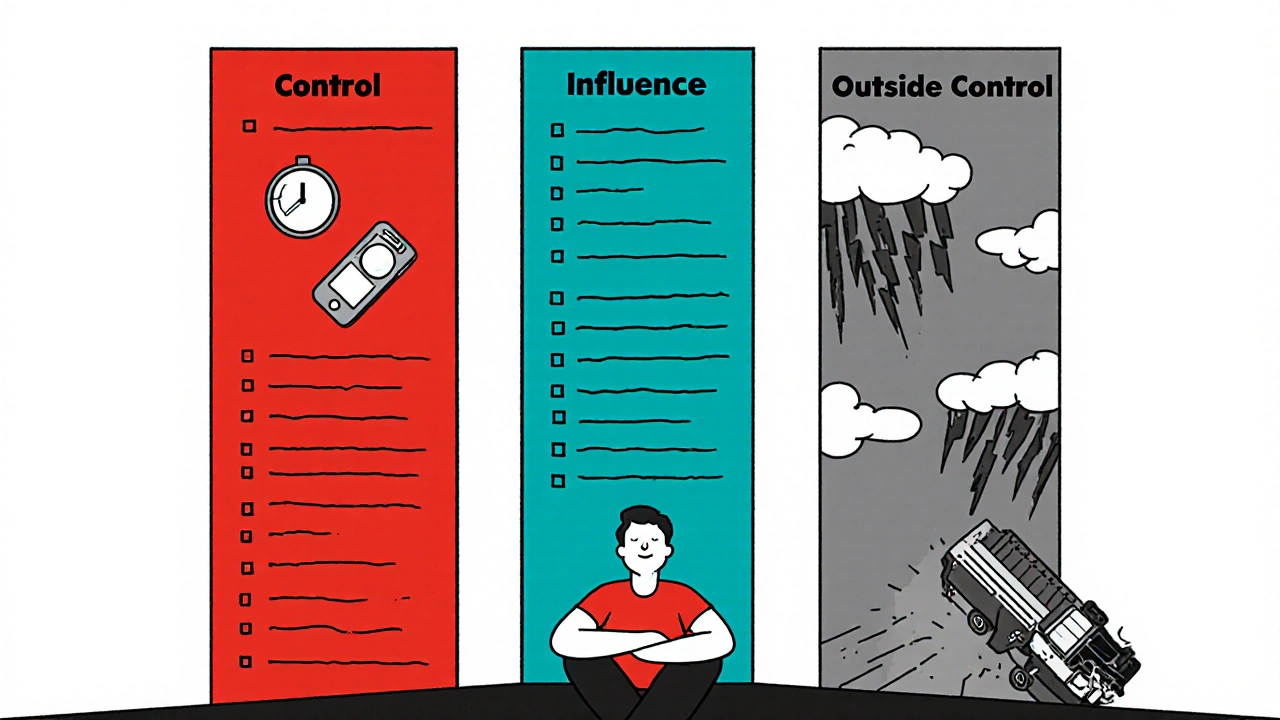
The most powerful tool you have during a transition isn’t an app or a calendar-it’s perspective. Research from Supportive Care’s 2023 analysis found that people who divided their concerns into three categories improved adherence by over 22%.- Things you can control directly: These are actions only you can take. Taking your pill. Calling your pharmacy. Writing down when you last took your dose. This category makes up just 27.3% of your stressors, but it’s where your energy should go.
- Things you can influence but not control: Your doctor’s availability, pharmacy hours, insurance delays. You can call, ask, advocate-but you can’t force a response. Spend time here only to reduce frustration, not to obsess.
- Things entirely outside your control: Your boss’s schedule, your ex’s behavior, a delayed moving truck. This is where most people waste mental energy. And it’s the biggest reason adherence fails.
Anchor Routines: The 3-5 Daily Non-Negotiables
You don’t need to keep your whole routine. You just need to keep a few anchors. A study in the Journal of Personality and Social Psychology found that people who maintained just 3 to 5 consistent daily activities during transitions reduced psychological distress by 23% and improved medication adherence by 31%. These aren’t big rituals. They’re tiny, repeatable moments that signal safety to your brain. Examples:- Take your morning pill right after brushing your teeth.
- Put your evening meds next to your coffee mug.
- Set a 10 p.m. alarm labeled “Meds & Breathe.”
Why Apps Alone Don’t Work (And What Does)
You might think a medication reminder app is the answer. And it is-until your life falls apart. General adherence apps show 23% better adherence during stable times. But during transitions? That advantage shrinks to just 8%. Why? Because they don’t adapt. They don’t ask, “Are you moving? Are you stressed? Are you alone?” The apps that do work during transitions-like TransitionAdhere and LifeShiftRx-are built differently. They include features like:- “Change Scenario” planners: “I’m moving next week. Help me adjust my routine.”
- Flexible reminders: “Take this pill within 4 hours of your last meal.”
- Emergency contacts: One tap to notify a friend or provider if you miss a dose.
Therapy Is a Medication Adherence Tool
Most people don’t think of therapy as a way to take their pills. But it is. Acceptance and Commitment Therapy (ACT), a form of cognitive behavioral therapy, has been shown to improve adherence by nearly 49% during life transitions, according to a 2022 JAMA Internal Medicine trial. ACT doesn’t try to eliminate stress. It teaches you to move forward with it. The core idea? You don’t need to feel motivated to take your meds. You just need to know why they matter-and choose to do it anyway, even when you’re tired, scared, or overwhelmed. A simple ACT exercise: Write down one reason your medication matters to you. Not “My doctor said so.” But something personal: “I want to be there for my kid’s graduation.” “I don’t want to end up back in the hospital.” “I want to walk my dog without feeling dizzy.” Keep that note on your phone. Read it before you take your pill. It reconnects you to your values when your routine is gone.Ask for Help-But Ask the Right Way
Social support is the single strongest predictor of adherence during stress. People with strong support networks have 42% lower cortisol levels and 34% better adherence, according to Health Psychology. But asking for help isn’t about saying, “Can you remind me to take my pills?” That’s a chore for someone else. It’s about asking for partnership. Try this:- “I’m going through a big change next month. My meds are important. Can we set up a quick call to figure out how you can help?”
- “I need someone to check in on me-not to nag, but to ask, ‘How’s your routine going?’”
- “I’m not asking you to manage this. Just to notice if I seem off.”
Work With Your Provider-Before the Crisis Hits
Your doctor should be part of your transition plan-not a last resort. The American College of Physicians now recommends that all providers screen for upcoming life changes during routine visits. Ask: “What’s coming up in the next few months?” Then say: “I’m worried my meds might slip. Can we make a plan?” A good provider will help you:- Switch to long-acting meds if daily dosing is too hard.
- Get a 90-day supply to reduce pharmacy trips.
- Set up automatic refills.
- Connect you with a pharmacist who specializes in transitions.
One Small Step at a Time
The biggest mistake? Trying to fix everything at once. During divorce, one woman broke her medication routine into tiny steps:- Week 1: Find a new pharmacy.
- Week 2: Get a pill case with compartments.
- Week 3: Link pills to her morning tea.
What to Do Right Now
If you’re facing a transition-or know one is coming-do this today:- Write your three lists: control, influence, outside your control.
- Identify your 3 daily anchors. Link them to existing habits.
- Download a transition-specific app (like LifeShiftRx) and set it up now.
- Write down one personal reason your medication matters. Save it on your phone.
- Call your doctor. Say: “I have a big change coming. Can we make an adherence plan?”
Why do I keep forgetting my meds during big life changes?
It’s not memory. It’s stress. When your life shifts-like moving, changing jobs, or ending a relationship-your brain goes into survival mode. Planning and routine tasks get pushed aside because your body is focused on handling the emotional and physical chaos. Your medication routine isn’t a priority right now, even if it’s important. The fix isn’t better reminders-it’s simpler, more flexible routines tied to things you can’t change, like brushing your teeth or eating breakfast.
Are pill organizers useless during transitions?
Not useless-but limited. Pill organizers work well when your schedule is stable. But during transitions, you might not be home every day, or you might be traveling, staying with someone, or just too overwhelmed to open the box. A better option is a digital app with flexible reminders or a 90-day prescription so you don’t need to refill often. If you use a pill organizer, keep it in your bag or car-not just on your kitchen counter.
Can I switch to a once-a-day pill to make things easier?
Yes-and you should ask your doctor about it. Many medications have extended-release versions or combination pills that reduce daily doses. For example, some blood pressure or antidepressant meds can be switched to once-daily forms. Reducing the number of times you need to remember a pill cuts adherence risk by nearly half. Don’t assume your current regimen is fixed. Talk to your provider about simplifying it before your transition hits.
I’m scared to tell my doctor I’ve missed doses. What should I say?
Say this: “I’ve been going through a big change, and I haven’t been able to take my meds like I should. I’m not proud of it, but I want to fix it.” Doctors hear this all the time. They’re not there to judge-they’re there to help you stay healthy. In fact, the American College of Physicians now encourages providers to proactively ask about transitions. If your doctor reacts negatively, it’s time to find one who understands how stress affects health.
How long does it take to rebuild a medication routine after a transition?
It takes 2 to 3 weeks to re-establish a new habit, but you don’t need to wait for “perfect.” Start with one anchor-like taking your pill after your first sip of coffee. Once that’s automatic, add another. Most people who succeed don’t rebuild everything at once. They rebuild one small piece at a time. The goal isn’t perfection. It’s progress. Even 80% adherence during a transition is better than 0%.
