Trigeminal Neuralgia Impact Calculator
Daily Activity Impact
Rate how much trigeminal neuralgia affects your daily routines:
Mental Health Impact
Rate your current mental health status:
Pain Intensity Scale
On a scale of 0-10, how would you rate your average daily pain level?
Your Trigeminal Neuralgia Impact Report
Activity Impact Score: 0
Mental Health Impact Score: 0
Pain Intensity: 5/10
Recommendations:
- Consider keeping a trigger journal to identify patterns
- Discuss mental health support with your healthcare provider
- Explore complementary therapies like meditation or physical therapy
When you hear the term Trigeminal Neuralgia is a chronic facial pain disorder that strikes the trigeminal nerve, delivering sudden, electric‑shock‑like attacks that can last from a split second to a few minutes. For many sufferers, those fleeting bursts turn everyday routines into a guessing game: will a sip of coffee or a breeze on the cheek trigger the next jolt? The ripple effect goes far beyond the face-it seeps into work, relationships, and even sleep.
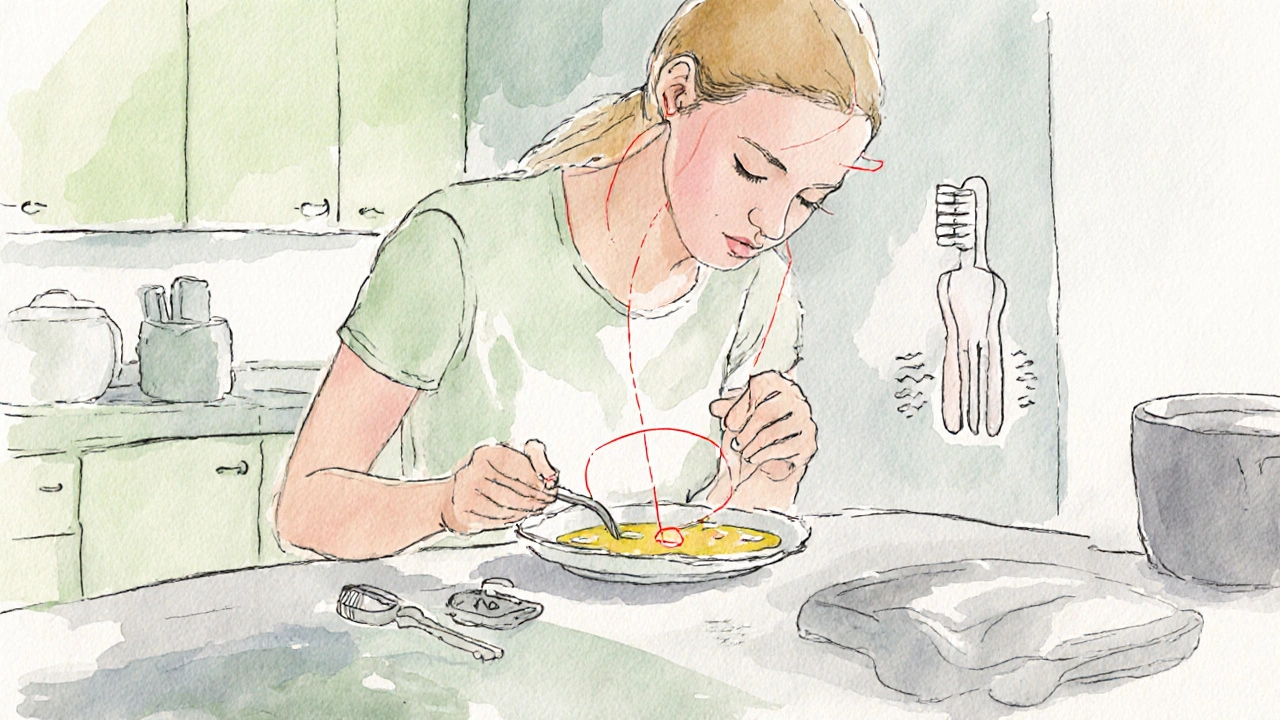
Daily Activities Turn into Minefields
Simple chores become tactical decisions. Brushing teeth, shaving, or even applying makeup can feel like walking through a field of land mines. The sudden onset of pain often forces people to change their grooming habits, avoid social gatherings, or skip meals that involve chewing. Over time, these compromises erode a sense of normalcy.
Driving is another hidden challenge. The act of pulling a hand‑brake or checking side mirrors can stimulate trigger zones on the face, leading to a painful episode mid‑journey. Many patients report limiting trips to short distances or relying on public transport to reduce exposure.
Workplace productivity suffers as well. A research survey from 2023 involving 1,200 patients showed that 68% missed at least one workday per month due to uncontrolled pain. Those who kept showing up often needed frequent breaks, which disrupted workflow and caused strain with colleagues.
When Pain Meets the Mind: Mental Health Consequences
Living with unpredictable pain creates a breeding ground for anxiety. The constant anticipation-"Will the next trigger happen now?"-activates the brain’s threat circuitry, raising cortisol levels and making sleep harder to achieve. In a longitudinal study conducted by the University of Oxford, 54% of participants with Anxiety reported that their condition aggravated the anxiety, creating a vicious loop.
Depression follows closely behind. The loss of hobbies, reduced social contact, and the feeling of helplessness can push patients into a low mood. A 2022 meta‑analysis of 18 studies found that 47% of people with Depression met criteria for moderate to severe depressive episodes, compared with 12% in the general population.
Quality of life, a broad metric that captures physical, emotional, and social well‑being, drops dramatically. The Quality of life scores for trigeminal neuralgia patients are often comparable to those living with terminal cancer, according to a 2024 European Neurology report.
Measuring the Invisible: Pain Scales and Their Limits
Clinicians usually rely on the Visual Analog Scale (VAS) to capture pain intensity. While VAS offers a quick snapshot-0 meaning no pain, 10 meaning worst imaginable-it cannot fully convey the episodic nature of trigeminal attacks, which may fluctuate wildly throughout a single day.
Because the pain is so brief, patients often report a low average VAS score even when the spikes are devastating. This mismatch can lead doctors to underestimate the condition’s impact, delaying aggressive treatment.
Treatment Landscape: What Works and When
Managing trigeminal neuralgia is a balancing act between symptom control and side‑effect tolerability. Below is a quick comparison of the most common options.
| Treatment | Success Rate | Main Risks | Typical Recovery |
|---|---|---|---|
| Carbamazepine | 70‑80% initial relief | Drowsiness, blood‑count changes | Immediate (days) |
| Microvascular Decompression | 85‑90% long‑term control | Infection, hearing loss | 4‑6 weeks |
| Radiofrequency Thermocoagulation | 60‑70% after 1‑year | Facial numbness, recurrence | 1‑2 weeks |
Carbamazepine remains the first‑line drug because it blocks the abnormal firing of the trigeminal nerve. However, many patients develop tolerance or side effects, prompting doctors to rotate to alternatives like oxcarbazepine or gabapentin.
When medication fails, surgical options enter the scene. Microvascular Decompression (MVD) involves relocating the blood vessel that presses on the nerve. Success rates are high, but the procedure requires a craniotomy, so it’s reserved for younger, healthier individuals.
For those who cannot undergo open surgery, Radiofrequency Thermocoagulation offers a minimally invasive alternative. By heating the nerve fibers under imaging guidance, clinicians can interrupt pain signals. The trade‑off is a higher chance of numbness around the face.
Living Strategies: Beyond Medicine
Even with optimal treatment, lifestyle tweaks can lessen the mental burden. Here are a few practical moves:
- Trigger journaling: Note the foods, temperatures, or facial movements that precede an attack. Over weeks, patterns emerge, allowing you to avoid or prep for high‑risk situations.
- Mind‑body practices: Techniques like progressive muscle relaxation or guided imagery have been shown to lower anxiety scores by up to 15% in chronic pain cohorts.
- Support networks: Joining a local or online trigeminal neuralgia group reduces isolation. Sharing coping tips often leads to new trigger‑avoidance ideas.
- Physical therapy: Gentle facial stretches, under a therapist’s guidance, can improve muscle balance and reduce pressure on the nerve.
Professional mental health support is equally vital. Cognitive‑behavioral therapy (CBT) equips patients with tools to reframe catastrophic thoughts about pain, which in turn can lower perceived pain intensity on the VAS.
When to Seek Help: Red Flags
If you notice any of the following, contact a neurologist promptly:
- Sudden increase in attack frequency or severity.
- New neurological symptoms such as weakness, numbness beyond the typical distribution, or vision changes.
- Side‑effects from medication that affect liver function or blood counts.
Early intervention can prevent the compounding of physical pain and mental distress, preserving both functional ability and quality of life.
Frequently Asked Questions
What triggers a trigeminal neuralgia attack?
Common triggers include light touch (e.g., shaving or applying makeup), temperature changes (hot or cold foods), wind, and even speaking. Individual triggers vary, so a personal diary is the best way to identify yours.
Is trigeminal neuralgia curable?
There is no permanent cure, but many patients achieve long‑term pain control with medication, surgery, or a combination of both. Ongoing research into nerve‑modulating devices offers hope for future solutions.
Can lifestyle changes reduce the frequency of attacks?
Yes. Avoiding known triggers, managing stress, and maintaining a balanced diet can lower attack frequency for many patients. Regular exercise and sleep hygiene also support overall neurological health.
What are the side effects of carbamazepine?
Common side effects include dizziness, drowsiness, nausea, and low blood cell counts. Rarely, it can cause serious skin reactions, so routine blood monitoring is essential.
How does trigeminal neuralgia affect mental health?
The unpredictable pain spikes trigger anxiety, while the chronic nature of the condition can lead to depression. Both are compounded by social isolation and the loss of everyday activities, making mental‑health support a key component of comprehensive care.
