Quitting smoking isn’t just about willpower. It’s about chemistry, behavior, and having the right tools. If you’ve tried quitting before and ended up back at the cigarette, you’re not alone. Most people need more than just determination. The science is clear: combining medication with support gives you the best shot at staying smoke-free for good.
What Actually Works to Quit Smoking?
Not all quit methods are created equal. Some feel like quick fixes. Others are backed by decades of research. The most effective approach isn’t one-size-fits-all, but there’s one medication that consistently comes out on top: varenicline (Chantix).
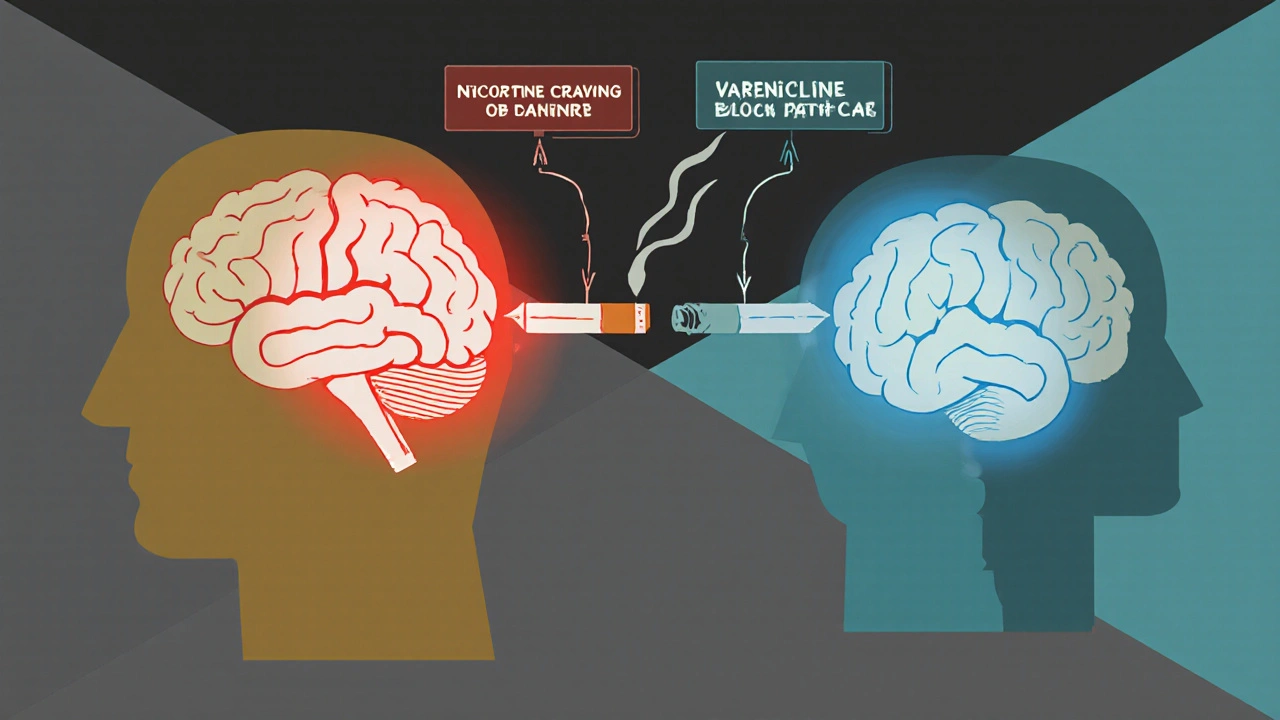
Developed by Pfizer and approved by the FDA in 2006, varenicline works differently than nicotine patches or gum. Instead of just replacing nicotine, it blocks the brain’s nicotine receptors. That means when you smoke, you don’t get the usual rush-and when you don’t smoke, your cravings are weaker. Clinical trials show it more than doubles your chances of quitting compared to a placebo. In the landmark EAGLES study, 21.8% of people using varenicline were still smoke-free after six months. That’s nearly twice the rate of those using a nicotine patch (15.7%) or bupropion (16.2%).
It’s not magic, though. Varenicline requires a 12-week course. You start with 0.5 mg once daily for three days, then bump up to 0.5 mg twice daily for four days, and finally 1 mg twice daily. You’re supposed to begin taking it 1 to 2 weeks before your quit date. That gives your brain time to adjust. The American Thoracic Society, the American Academy of Family Physicians, and the CDC all recommend it as a first-line treatment. Even people with depression or anxiety respond better to varenicline than to other options.
How Other Medications Compare
Not everyone can or wants to take varenicline. That’s where other options come in.
Nicotine Replacement Therapy (NRT) includes patches, gum, lozenges, nasal sprays, and inhalers. These deliver nicotine without the tar and carbon monoxide from cigarettes. Patches give steady nicotine levels. Gum and lozenges kick in fast when a craving hits. The CDC recommends using a combination-like a patch plus gum-for people who smoke more than 10 cigarettes a day. Studies show NRT gets you to about 10-16% success at six months. It’s safer than prescription meds, available over the counter, and often cheaper. But it’s less effective than varenicline. One analysis found varenicline was 32% more effective than standard NRT.
Bupropion (Zyban) was originally an antidepressant. It was later found to reduce nicotine cravings and withdrawal symptoms. It’s taken as a 150 mg tablet once daily for three days, then twice daily starting a week before your quit date. The EAGLES trial showed 16.2% of users were smoke-free after six months. People with depression often report improved mood while taking it. But it’s not for everyone. Some get insomnia, dry mouth, or even seizures (rare, but real). It’s also less effective than varenicline-about 46% less so, according to the same meta-analysis.
There’s also cytisine, a plant-based compound from Bulgaria and Eastern Europe. It works like varenicline but costs a fraction of the price. Early studies suggest it might be just as effective. The FDA hasn’t approved it yet, but it’s gaining attention. In a 2024 meta-analysis, it showed higher continuous abstinence rates than varenicline in some populations. If it gets approved in the U.S., it could be a game-changer for low-income smokers.
Combination Therapy: The Hidden Secret
The best results don’t come from one drug alone. They come from stacking them.
A 2022 network meta-analysis found that combining varenicline with NRT (like a patch plus gum) boosted quit rates dramatically. The odds of staying smoke-free went up by 5.75 times compared to placebo. That’s not a small bump-it’s a massive leap. The U.S. Public Health Service guidelines say this combination is safe and effective. Many doctors don’t mention it because they’re used to prescribing one thing at a time. But if you’re serious about quitting, ask about combining varenicline with a fast-acting NRT.
Real-world data backs this up. A 2022 Consumer Reports survey of over 1,200 ex-smokers found that 58% succeeded with varenicline alone, but 67% succeeded with varenicline plus NRT. The key is timing. Take the patch daily for steady control. Use gum or lozenges when cravings hit hard. Don’t wait until you’re desperate. Start using them as soon as you feel the urge.

Side Effects and Real-Life Challenges
Nothing works if you stop taking it. And many people do.
Varenicline’s most common side effect is nausea-about 30% of users report it. It usually fades after a week or two. Taking it with food helps. Vivid dreams or strange sleep patterns affect about 40% of users. That’s enough for 15% to quit the medication. Bupropion can cause insomnia or anxiety. NRT can cause jaw pain (gum), throat irritation (lozenges), or skin redness (patches).
But here’s what the data doesn’t tell you: most side effects aren’t dangerous. Early fears about varenicline causing depression or suicidal thoughts were based on anecdotal reports. The EAGLES trial, the largest study ever done on psychiatric safety, found no increased risk-even in people with a history of mental illness. The FDA removed its black box warning in 2016. Still, stigma lingers. Some doctors hesitate to prescribe it. Don’t let that stop you. Talk to your provider. Ask for the evidence.
Adherence is the real enemy. Only 44% of people finish the full 12-week course. Cost is a big reason. Without insurance, varenicline runs about $500 for 12 weeks. Bupropion is cheaper-around $15 for 30 days at Walmart’s $4 generic list. NRT patches cost $45 for a week’s supply at Walgreens. If you’re on Medicaid, coverage varies by state. In non-expansion states, only 29% of beneficiaries get access. If cost is a barrier, ask about patient assistance programs. Pfizer offers discounts for varenicline. Many pharmacies have loyalty programs. And don’t forget: quitting smoking saves you hundreds a month. That money can pay for the meds.
Behavioral Support: The Missing Piece
Medication alone isn’t enough. You need to rewire your habits.
Smoking isn’t just about nicotine. It’s tied to coffee, driving, stress, socializing, boredom. If you don’t change those triggers, you’ll relapse. That’s where counseling comes in. Even a 3-minute chat with your doctor increases your chances of quitting by 30%. Four or more sessions with a counselor? That pushes success rates to 60% or higher when combined with medication.
You don’t need fancy therapy. Free options exist. The CDC’s 1-800-QUIT-NOW hotline connects you to coaches. Smokefree.gov offers text message programs. Apps like QuitGuide and MyQuit Coach track cravings and give tips. Reddit’s r/stopsmoking community has over a million members sharing real stories. One user wrote: “Varenicline cut my cravings in half. But I only stayed quit because I started walking after dinner instead of lighting up.” That’s the secret. Replace the habit, don’t just fight the craving.
Who Should Use What?
There’s no perfect choice for everyone. But here’s a simple guide:
- If you want the highest success rate → Start with varenicline. Add NRT if cravings are strong.
- If you have depression or anxiety → Varenicline is still best. Bupropion can help mood, but varenicline works better overall.
- If you can’t afford prescriptions → Use NRT (patch + gum). It’s cheaper and available without a script.
- If you’ve tried everything and failed → Try combination therapy. Or ask about cytisine if it becomes available.
- If you’re under 25 → You’re less likely to use medication. But you’re also more likely to succeed with support. Use apps, quitlines, and peer groups.
Black smokers, who often respond poorly to NRT and bupropion, benefit the most from varenicline. Studies show they’re 50-70% more likely to quit with it than with other options. This isn’t a coincidence-it’s science.
What to Do Next
Ready to quit? Here’s your action plan:
- Set a quit date-within the next two weeks.
- Call 1-800-QUIT-NOW or visit Smokefree.gov. Get a free coach.
- Ask your doctor for varenicline. If it’s too expensive, ask about bupropion or NRT.
- Start your medication 1-2 weeks before your quit date.
- Use fast-acting NRT (gum or lozenge) for breakthrough cravings.
- Identify your top three triggers (coffee, stress, driving) and plan a replacement (drink water, take a walk, chew gum).
- Don’t give up if you slip. Most people try 3-5 times before quitting for good.
Quitting isn’t a one-time event. It’s a process. The first week is the hardest. The first month is tough. But after three months, your brain starts healing. Cravings fade. Your lungs clear. Your sense of taste comes back. And the money you save? That’s real freedom.
Is varenicline safe if I have depression?
Yes. Early concerns about varenicline causing depression or suicidal thoughts were based on limited reports. The EAGLES study, which included over 8,000 people with psychiatric conditions, found no increase in serious mood-related side effects compared to placebo. The FDA removed its black box warning in 2016. Varenicline is now recommended as a first-line treatment even for people with depression or anxiety.
Can I use nicotine gum and a patch together?
Yes, and it’s often more effective than using either alone. The CDC recommends combining a long-acting patch (21mg) with a fast-acting form like gum or lozenges for breakthrough cravings. This mimics the way people smoke-steady background nicotine plus quick hits. Use the patch daily. Use gum or lozenges when you feel the urge, up to 1-2 per hour. Don’t exceed 20 pieces of gum a day.
How long do I need to take varenicline?
The standard course is 12 weeks. But if you’re still smoke-free after that, your doctor may recommend continuing for another 12 weeks. Studies show that people who take it longer have lower relapse rates. Don’t stop just because you’ve made it to week 12. Stay on it if you’re doing well. The goal is to rewire your brain, not just survive the first month.
What if I relapse after quitting?
Relapse doesn’t mean failure. Most people try to quit multiple times before succeeding. If you smoke again, don’t blame yourself. Figure out what triggered it-stress? Social pressure? Boredom? Then adjust your plan. You might need stronger medication, more counseling, or different coping strategies. Many people who relapse go back on varenicline and quit successfully the second time. It’s not about perfection. It’s about persistence.
Are over-the-counter quit aids as good as prescriptions?
Not quite. NRT (patches, gum, lozenges) works, but it’s less effective than varenicline or bupropion. About 10-16% of people quit with NRT alone. With varenicline, that number jumps to 20-22%. The difference is significant. But if you can’t get a prescription, NRT is still better than nothing. Combine it with free counseling or apps to boost your odds. And remember: even small success rates add up when millions of people use them.