Medication Interaction Checker
Check Your Medications
Enter your current medications to check for dangerous interactions and ingredient overlaps.
Every winter, millions of people grab a bottle of cold medicine without reading the label. They think they’re doing the right thing-taking something to feel better. But what they don’t realize is that they might be mixing dangerous chemicals without even knowing it. The problem isn’t just one pill. It’s stacking them. Combining allergy meds with cold meds. Adding painkillers on top. And ending up in the ER because they didn’t check what was already inside their medicine cabinet.
Why Combination Medications Are a Trap
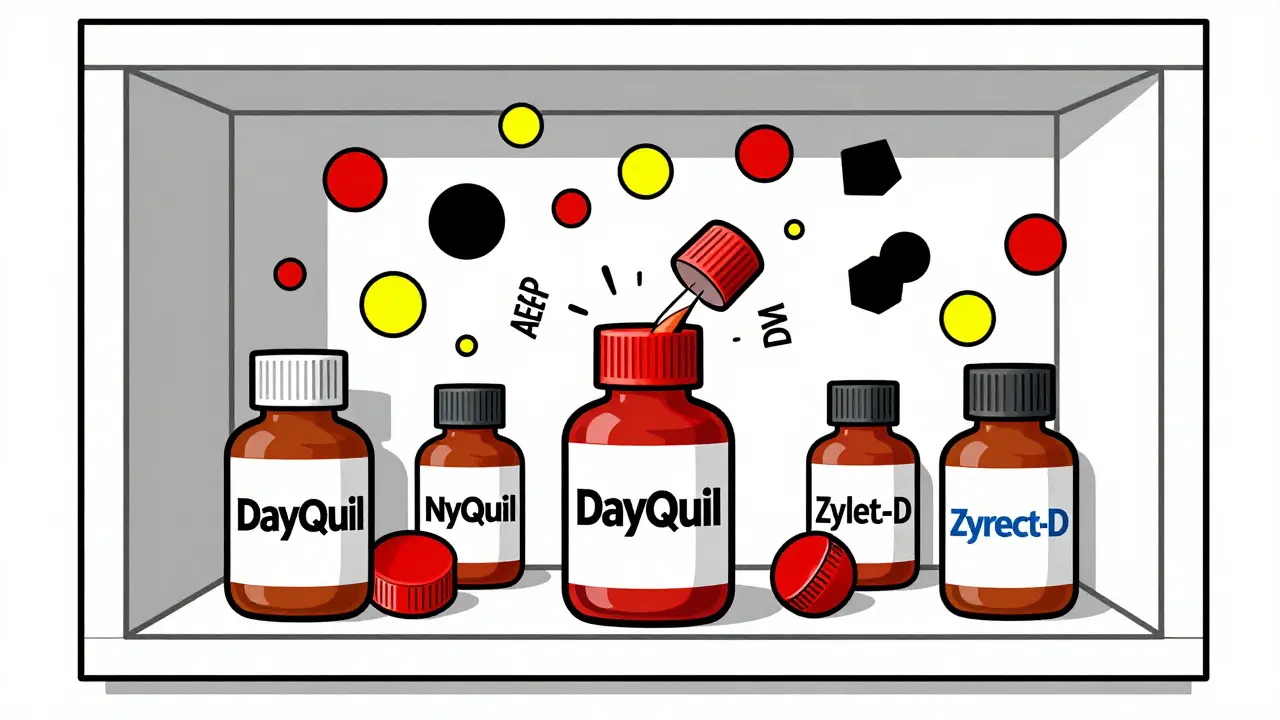
Most cold and allergy meds you find on the shelf aren’t just one drug. They’re a cocktail. Take DayQuil, NyQuil, or Tylenol Sinus. Each contains at least two, often three or four active ingredients. You get an antihistamine for runny nose, a decongestant for stuffiness, an analgesic for headache, and a cough suppressant for that nagging cough. Sounds convenient, right? That’s the whole point. But convenience comes with hidden risks. The FDA says about 65% of all cold and allergy meds sold in the U.S. are combination products. That’s over 300 million bottles a year. And here’s the scary part: these products cause 23% more adverse reactions than single-ingredient ones. Why? Because people don’t realize they’re doubling up. For example, you take Tylenol Cold & Flu for your fever and sore throat. Later, you take a separate Tylenol tablet for a headache. You’re now at 1,000 mg of acetaminophen in one dose-double what’s safe if you’ve already hit your limit. Acetaminophen, also labeled as APAP on bottles, is the most common cause of accidental liver failure in the U.S. The FDA limits daily intake to 4,000 mg, but it’s easy to go over when you’re juggling three different meds-all with acetaminophen inside.The Silent Killer: Acetaminophen in Everything
You won’t find acetaminophen listed as “acetaminophen” on every label. Look for APAP. That’s the abbreviation. And it’s hiding in more than half of all combination cold and allergy products. A 2022 CDC study found that 6.7 million Americans accidentally overdose on acetaminophen every year-almost all from mixing meds. It doesn’t take much. One 500 mg tablet of regular Tylenol. One caplet of DayQuil. One tablet of Theraflu. That’s 1,500 mg before lunch. Add a nighttime cold med with acetaminophen? You’re at 2,500 mg by bedtime. Do that for three nights? You’re over the safe limit. And your liver doesn’t scream until it’s too late. The worst part? Most people don’t know what they’re taking. A Consumer Reports survey found that 41% of adults never check all the ingredients on OTC labels. They see “cold medicine” and assume it’s safe. They don’t know APAP = acetaminophen. They don’t know that NyQuil and Zyrtec-D both contain pseudoephedrine. They don’t know that taking both could spike their blood pressure.Decongestants: The Hidden Heart Risks
Pseudoephedrine and phenylephrine are the two main decongestants in cold meds. One works. The other? Maybe not. Pseudoephedrine (found in Sudafed) is proven to shrink nasal passages. It reduces congestion by 65%. But it also raises your blood pressure by 8-12 mmHg and increases heart rate by 5-8 beats per minute. If you have high blood pressure, heart disease, or an overactive thyroid, this can be dangerous. The FDA warns against using it if your systolic pressure is over 180 or diastolic over 110. Phenylephrine (in Tylenol Sinus, Sudafed PE) is everywhere now. Why? Because pseudoephedrine is kept behind the counter due to its use in making meth. But here’s the truth: multiple clinical trials show that 10 mg of oral phenylephrine does nothing better than a placebo. It doesn’t relieve congestion. Yet it’s still in 30% of all cold products. And here’s the kicker: when phenylephrine is mixed with acetaminophen, your body absorbs four times more of it. That’s not a typo. A 2014 study in the Journal of Clinical Pharmacology proved this. So you’re not just getting a useless decongestant-you’re getting a stronger, riskier version of it. That means higher chances of dizziness, rapid heartbeat, or even stroke in vulnerable people.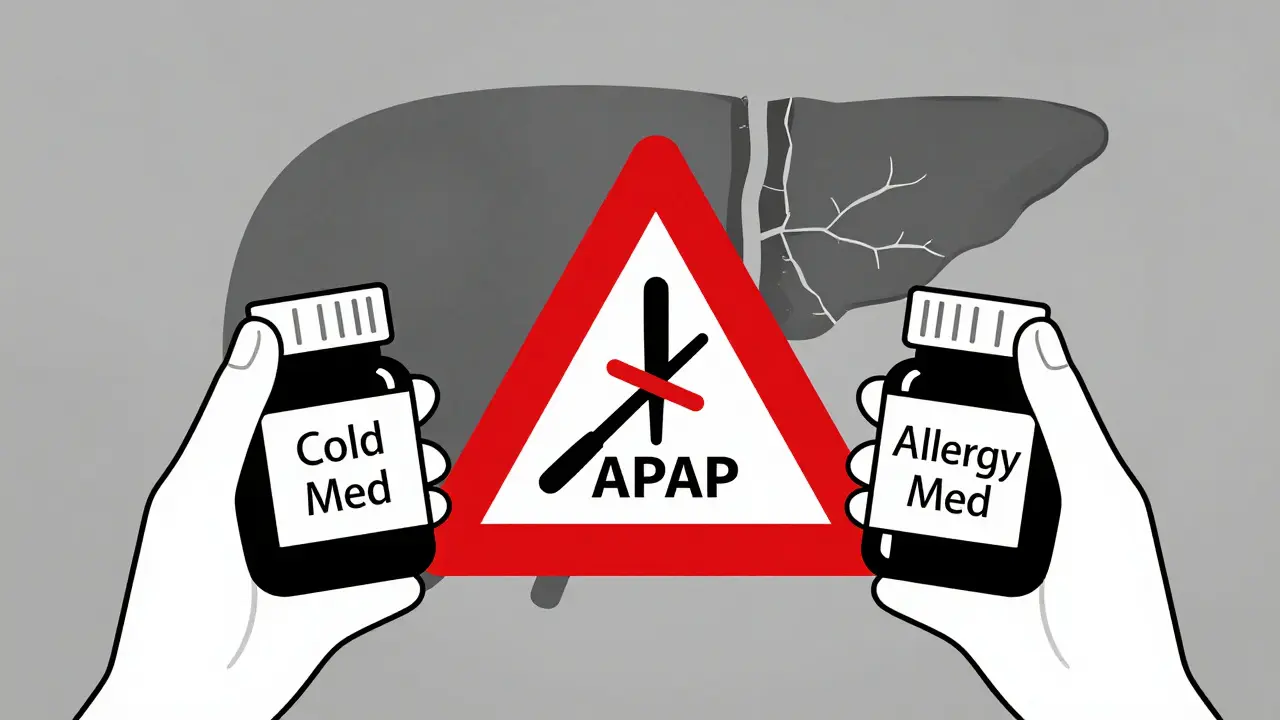
Dextromethorphan and Antidepressants: A Dangerous Mix
Dextromethorphan (DM) is the cough suppressant in Robitussin, Coricidin, and many others. It’s safe when taken alone. But combine it with antidepressants-especially SSRIs like Prozac, Zoloft, or SNRIs like Cymbalta-and you’re playing Russian roulette. This combo can trigger serotonin syndrome. It’s rare, but deadly. Symptoms include confusion, high fever, fast heartbeat, muscle stiffness, seizures. A 2017 study in the Journal of Clinical Psychiatry found the risk jumps 300% when dextromethorphan is taken with these drugs. And people don’t even realize they’re at risk. They take their antidepressant daily. They get a cold. They grab a bottle of cough syrup. They don’t think twice. Desert Hope Treatment Center reports that 15% of emergency visits from OTC misuse involve cold meds mixed with antidepressants. These aren’t recreational users. These are regular people trying to feel better.What You Should Do Instead
Stop grabbing the multi-symptom bottle unless you have ALL the symptoms. If you only have a stuffy nose? Get a plain decongestant. Only a cough? Use plain dextromethorphan. Only a headache? Stick with plain acetaminophen or ibuprofen. Here’s how to do it right:- Read every label. Look for active ingredients. Not just the brand name.
- Check for duplicates. If you’re taking two products, make sure they don’t share the same active ingredient.
- Know the abbreviations. APAP = acetaminophen, DM = dextromethorphan, PE = phenylephrine, PSE = pseudoephedrine, CL = chlorpheniramine, DP = diphenhydramine.
- Use a drug checker. Apps like Medisafe or WebMD’s interaction checker scan your meds and flag conflicts. They process over a million checks daily.
- Ask a pharmacist. They’re trained to spot these mistakes. Take your bottle in. Say: “I’m taking this with my regular meds. Is it safe?”