DOAC Safety Selector Tool
Select Your Profile
This tool helps you understand the relative bleeding risks of apixaban, rivaroxaban, and dabigatran based on your medical factors.
Choosing a blood thinner isn’t just about picking the most popular one. With apixaban, rivaroxaban, and dabigatran - three of the most common direct oral anticoagulants (DOACs) - the differences in side effects can be life-changing. You might think they’re all the same: no need for regular blood tests, fewer food interactions than warfarin. But the truth is, apixaban has a distinct safety profile that makes it the preferred choice for many patients, especially those at higher risk of bleeding.
Why GI Bleeding Matters More Than You Think
Gastrointestinal bleeding isn’t just a side effect - it’s often the deciding factor in which drug a doctor picks. If you’ve had a stomach ulcer, take NSAIDs for arthritis, or are over 70, this isn’t just a footnote - it’s a red flag. Data from the JAMA Network in 2022 showed rivaroxaban caused nearly twice as many GI bleeds as apixaban: 35.2 events per 1,000 patient-years versus 16.3. That’s not a small difference. It’s a 200% higher risk. Dabigatran wasn’t far behind, with rates close to rivaroxaban’s. But apixaban? It consistently comes out on top. Multiple studies, including one from Oxford Academic and another in the Annals of Internal Medicine, confirm this pattern across age groups, kidney function levels, and even in patients on aspirin or other painkillers. Why does this happen? It’s not fully understood, but it’s likely tied to how these drugs interact with the gut lining. Dabigatran and rivaroxaban may irritate the stomach more directly. Apixaban, on the other hand, seems to pass through with less local effect. For someone with a history of bleeding ulcers, choosing apixaban over the others isn’t just cautious - it’s often the only safe option.Major Bleeding: Rivaroxaban’s Hidden Risk
When doctors talk about “major bleeding,” they mean bleeding that requires a hospital visit, transfusion, or causes a drop in hemoglobin. This isn’t a nosebleed - it’s internal, potentially fatal bleeding. Rivaroxaban stands out here too. The same JAMA study found 39.7 major extracranial bleeds per 1,000 patient-years with rivaroxaban. Apixaban? Just 18.5. That’s a 21% absolute difference - meaning for every 100 people on rivaroxaban for a year, about 4 more will have a serious bleed than if they were on apixaban. Even when compared to dabigatran, rivaroxaban shows higher rates. A 2012 analysis in JACC found apixaban had a 34% lower risk of major bleeding than rivaroxaban. And that’s not just in trials - this holds up in real-world data from tens of thousands of patients. If you’re older, have high blood pressure, or take other medications that affect bleeding, this isn’t a theoretical concern. It’s a real, measurable danger.Intracranial Hemorrhage: The One Place Rivaroxaban Might Be Better
Here’s where things get surprising. While rivaroxaban has higher GI and major bleeding risks, it might actually be slightly better at preventing the most dangerous kind of bleed: bleeding inside the skull. A 2022 study published in PubMed found rivaroxaban had a lower rate of intracranial hemorrhage than apixaban (hazard ratio 0.86). That’s a small but statistically significant difference. It’s the only area where rivaroxaban edges out apixaban in safety. But don’t get the wrong idea. All three DOACs are far safer than warfarin when it comes to brain bleeds. The real takeaway? If you’re at high risk for a stroke and also have a history of falls or brain aneurysms, your doctor might consider rivaroxaban - but only after weighing its higher GI and body-wide bleeding risks. For most people, the trade-off isn’t worth it.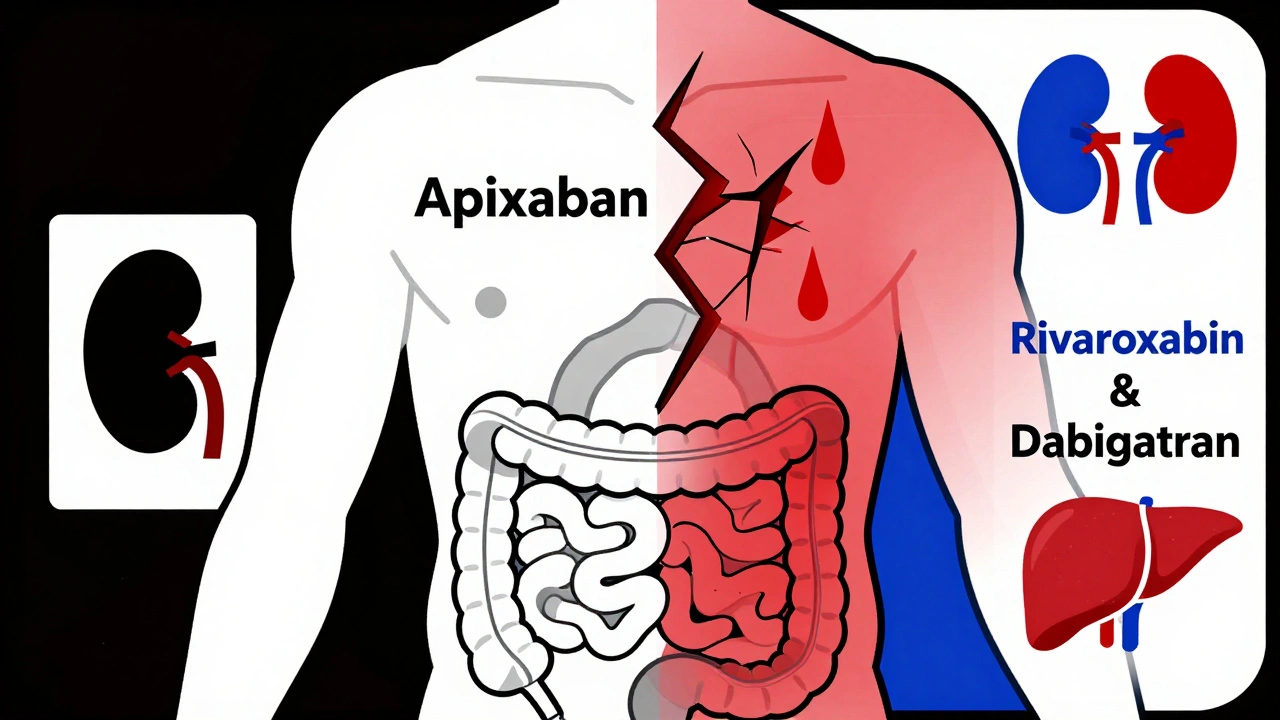
Dabigatran and the Heart Attack Question
Dabigatran has another unique risk: it might increase your chance of a heart attack or acute coronary syndrome. Multiple meta-analyses, including one from the PMC in 2014 and another in JACC, found a 48% higher relative risk of heart attack with dabigatran compared to other DOACs. The mechanism isn’t clear. Some researchers think it’s because dabigatran blocks thrombin - a key enzyme in clotting - but thrombin also plays a role in calming inflammation. Blocking it too much might trigger plaque rupture in arteries. It’s similar to what happened with ximelagatran, a drug pulled from the market for the same reason. If you have coronary artery disease, a history of heart attack, or angina, dabigatran may not be the best fit. Even if you’re healthy now, this risk adds up over time. For patients with atrial fibrillation and no heart disease, the risk is lower - but still present. That’s why many cardiologists avoid dabigatran in patients with known coronary issues.Dosing, Kidneys, and Daily Life
It’s not just about bleeding. How you take the drug matters too. Dabigatran requires two doses a day - no exceptions. It also clears mostly through the kidneys (80%). If your kidney function drops below 30 mL/min, you can’t take the higher dose. Below 15 mL/min? You can’t take it at all. That’s a big deal for older adults, who often have declining kidney function. Rivaroxaban is once-daily for stroke prevention - a big plus for adherence. But it’s still cleared by the kidneys (33%), and you can’t use it if your creatinine clearance is below 15 mL/min. Apixaban? Twice-daily, like dabigatran. But it’s cleared mostly by the liver (75%), with only 25% going through the kidneys. That makes it safer in mild to moderate kidney disease. It’s also the only DOAC still approved at full dose for patients with creatinine clearance as low as 15 mL/min - as long as they’re not on dialysis. For someone with chronic kidney disease, apixaban is often the only DOAC you can use without dose reduction or switching back to warfarin.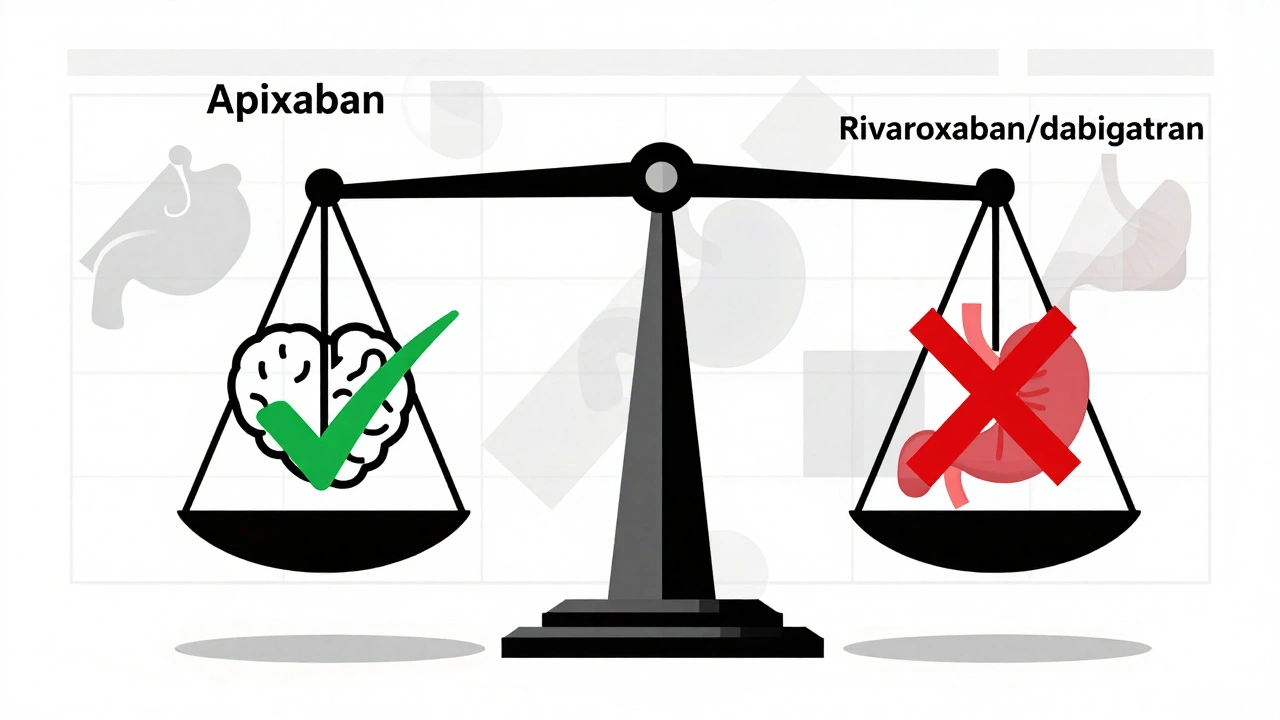
Who Gets Which Drug - And Why
So who gets what? Here’s how it breaks down in real practice:- Apixaban is the go-to for patients with a history of GI bleeding, older adults (especially over 80), those with kidney problems, or anyone on NSAIDs. It’s now the most prescribed DOAC in the U.S., making up nearly half the market.
- Rivaroxaban is often chosen for patients who struggle with twice-daily dosing - but only if they have no GI issues, no heart disease, and healthy kidneys. Its once-daily schedule helps with adherence, but the bleeding risk is real.
- Dabigatran is falling out of favor. It’s still used in young, healthy patients with no heart disease and perfect kidney function - but even then, many doctors now avoid it because of the heart attack risk and higher GI bleeding.
What’s Next?
New studies are coming. The AUGUSTUS-2 trial and ANTICOAG-CKD trial are looking at DOACs in high-risk groups - like those with severe kidney disease or on multiple blood thinners. There’s also early research into genetic testing that might predict who responds better to one DOAC over another. In the future, your DNA might help pick your blood thinner. For now, the evidence is clear: not all DOACs are created equal. Apixaban has the most favorable safety profile overall - especially for bleeding. Rivaroxaban’s convenience comes with a cost. Dabigatran’s risks are growing harder to ignore. If you’re on one of these drugs, ask your doctor: “Is this the safest choice for me, given my health history?” Don’t assume they’re all the same. Your life might depend on the difference.Which blood thinner has the least bleeding risk?
Apixaban has the lowest risk of gastrointestinal and major bleeding among the three main DOACs. Studies consistently show it causes about half the number of GI bleeds compared to rivaroxaban and dabigatran. It’s also safer in patients with kidney disease and older adults. For most people, especially those with prior bleeding or stomach issues, apixaban is the safest choice.
Can I switch from rivaroxaban to apixaban safely?
Yes, switching is common and generally safe when done under medical supervision. Doctors often switch patients from rivaroxaban to apixaban if they’ve had a GI bleed, are over 75, or have declining kidney function. The transition is usually done by stopping rivaroxaban and starting apixaban the next day - no overlap or bridging needed. Always consult your doctor before switching - timing matters to avoid clotting or bleeding risks.
Why is dabigatran less commonly prescribed now?
Dabigatran is used less because of two key risks: higher rates of gastrointestinal bleeding and a potential increase in heart attacks. Multiple large studies have shown it causes more stomach bleeds than apixaban and carries a 48% higher relative risk of heart attack compared to other DOACs. It also requires twice-daily dosing and is heavily cleared by the kidneys, making it risky for older or kidney-impaired patients. As safer alternatives like apixaban became available, prescribing shifted away from dabigatran.
Is apixaban better than warfarin?
Yes, apixaban is generally better than warfarin. It has a lower risk of intracranial bleeding, doesn’t require regular blood tests, has fewer food and drug interactions, and is just as effective at preventing strokes in atrial fibrillation. Clinical trials like ARISTOTLE showed apixaban reduced major bleeding by 31% and lowered death rates compared to warfarin. For most patients, apixaban is the preferred option over warfarin.
Do DOACs cause liver damage?
Liver damage from DOACs is extremely rare. Unlike some older blood thinners, apixaban, rivaroxaban, and dabigatran are not known to cause significant liver toxicity. A small number of cases of elevated liver enzymes have been reported, but these are uncommon and usually mild. If you have severe liver disease (Child-Pugh C), DOACs aren’t recommended - but not because they damage the liver. It’s because the body can’t process them properly, increasing bleeding risk. Routine liver tests aren’t needed unless you have existing liver disease.
If you’re managing atrial fibrillation or a blood clot, your medication isn’t just a pill - it’s a personalized tool. The differences between apixaban, rivaroxaban, and dabigatran aren’t academic. They’re real, measurable, and can change your outcomes. Ask questions. Demand data. And don’t accept “they’re all the same” as an answer.
