More than 32 million Americans live with osteoarthritis. That’s about one in four adults. And while many assume all joint pain is just "wear and tear," the truth is far more complex. Two of the most common types - osteoarthritis and rheumatoid arthritis - aren’t just different in symptoms. They’re different in cause, treatment, and long-term impact. Get the wrong diagnosis, and you could be missing critical care that stops damage before it’s permanent.
What Is Osteoarthritis? The Slow Burn of Joint Wear
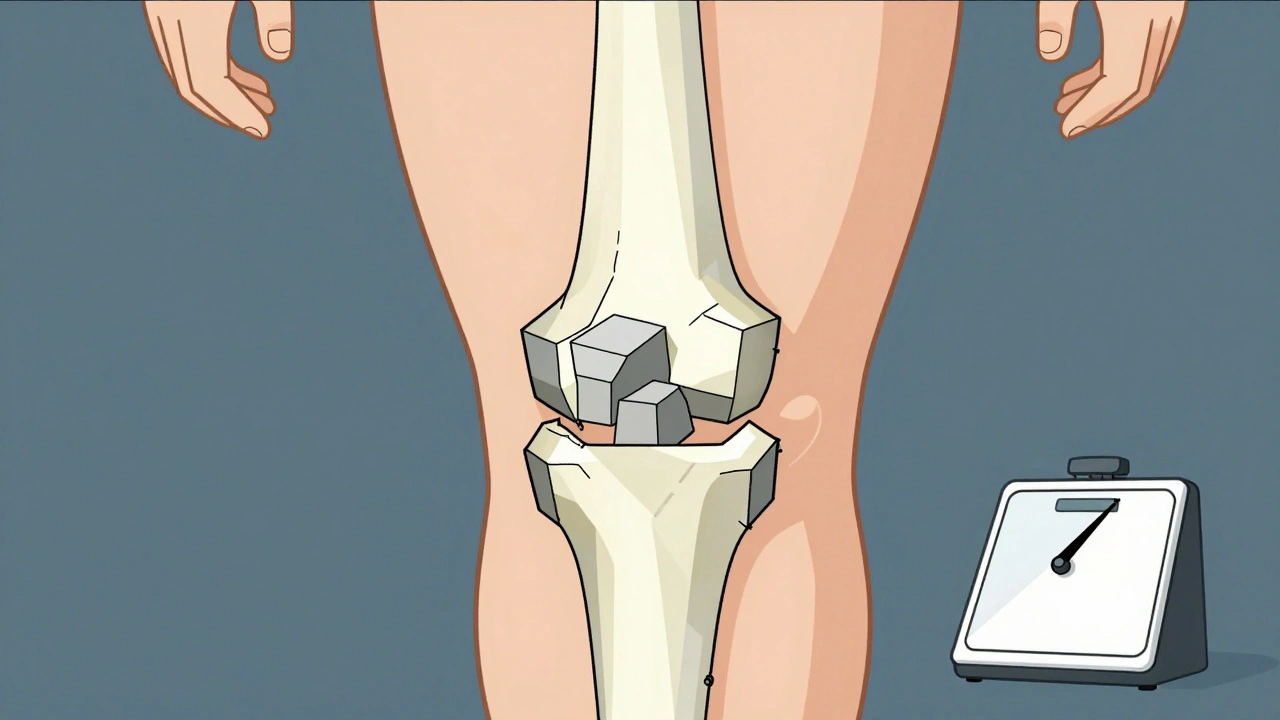
Osteoarthritis (OA) isn’t an illness you catch. It’s the result of your joints breaking down over time. Think of it like the cushioning in your shoes wearing thin. The cartilage - the smooth, slippery tissue that lets bones glide over each other - starts to fray. Eventually, bone rubs on bone. That’s when pain, stiffness, and swelling show up.
It usually hits the joints that carry weight or get repeated use: knees, hips, lower back, and hands. You’ll notice it most when you move. Climb stairs? Your knees ache. Grip a coffee mug? Your fingers stiffen. Morning stiffness? It’s brief - usually under 30 minutes. Unlike other types, OA doesn’t make you feel sick all over. No fevers. No fatigue. Just localized pain that gets worse with activity and improves with rest.
The biggest risk factor? Age. After 50, your chances rise sharply. But it’s not just aging. Obesity plays a huge role. Carrying extra weight puts pressure on your knees. Losing just 5 kilograms can cut knee pain in half. Genetics matter too. If your parents had hand OA, you’re more likely to develop it, especially in the DIP joints - the ones closest to your fingertips.
Diagnosis is straightforward. An X-ray shows narrowing joint space, bone spurs, or loss of cartilage. Blood tests come back normal. That’s key. If your blood shows inflammation markers, it’s probably not OA.
What Is Rheumatoid Arthritis? When Your Immune System Turns Against You
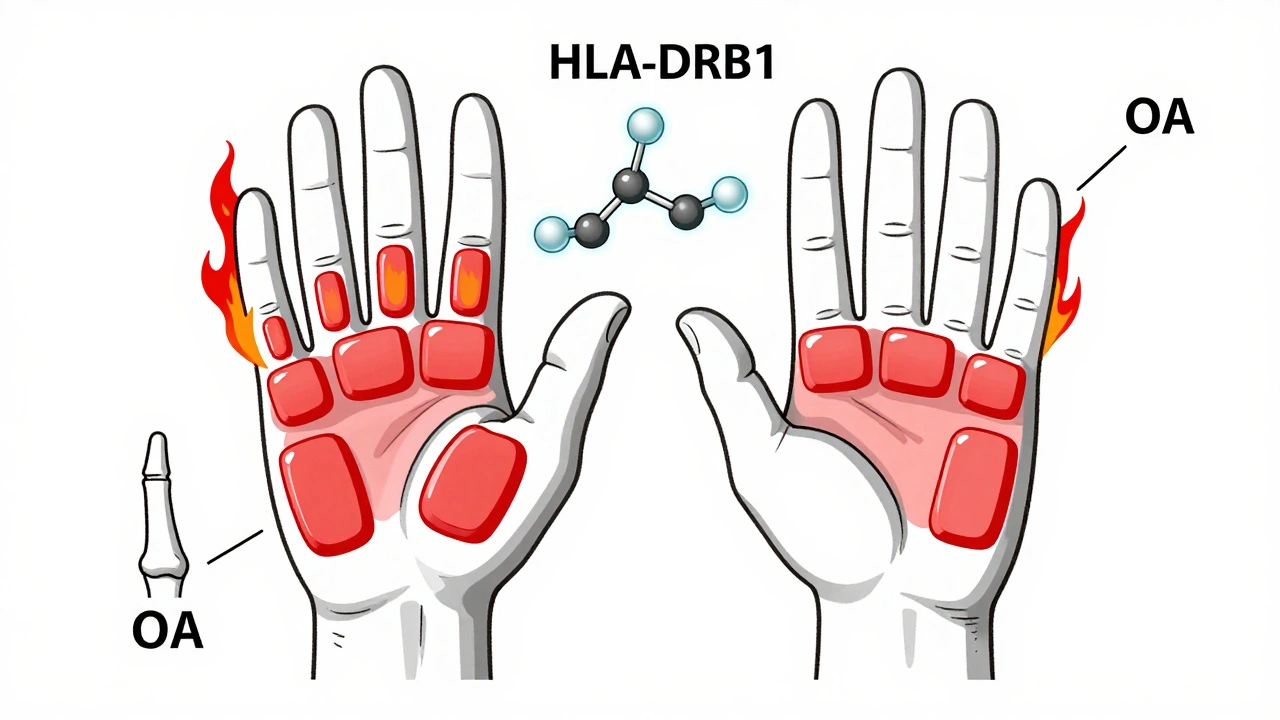
Rheumatoid arthritis (RA) is the opposite of OA. It’s not about wear and tear. It’s about your body attacking itself. Your immune system - the team that fights off viruses - mistakes the lining of your joints (the synovium) for an invader. It floods the area with inflammatory chemicals. The joint swells. The lining thickens. Over time, it eats away at cartilage and bone.
RA doesn’t wait for you to get old. It can strike in your 30s, 40s, or even earlier. Juvenile RA affects kids under 16. Women are three times more likely to get it than men. Smoking? That’s a major red flag. Smokers have two to three times higher risk. If you have the HLA-DRB1 gene variant, your chances go up even more.
Here’s what sets RA apart:
- Symmetrical pain: If your left wrist hurts, your right one will too. Both hands, both knees - always both sides.
- Long morning stiffness: You might be stuck in bed for over an hour, unable to move your fingers or stand up straight.
- Systemic symptoms: Fatigue. Low fevers. Weight loss. You feel like you’ve got the flu - but it doesn’t go away.
- Joint pattern: RA targets the MCP joints (knuckles) and wrists. It rarely touches the very tip of your fingers (DIP joints), unlike OA.
Diagnosis isn’t just about X-rays. Blood tests are critical. Rheumatoid factor (RF) and anti-CCP antibodies show up in most people with RA. But even if those tests are negative, you can still have RA - doctors look at symptoms, joint swelling, and imaging like ultrasound to confirm.
And here’s the hard truth: if RA isn’t treated within the first 3 to 6 months, joint damage can happen fast - sometimes in just weeks. That’s why early diagnosis saves function.
How They’re Different: Side-by-Side Comparison
| Feature | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Primary Cause | Mechanical wear and tear | Autoimmune attack on joint lining |
| Typical Onset Age | Over 50 | Any age, often 30-60 |
| Joint Symmetry | Often one-sided | Always symmetrical |
| Morning Stiffness | Less than 30 minutes | More than 60 minutes |
| Systemic Symptoms | None | Fatigue, fever, weight loss |
| Commonly Affected Joints | Knees, hips, spine, DIP fingers | Wrists, MCP knuckles, PIP fingers |
| Diagnosis Tools | X-ray, physical exam | Blood tests (RF, anti-CCP), ultrasound, clinical symptoms |
| Treatment Focus | Pain relief, joint protection, weight loss | Immunosuppression, DMARDs, biologics |
| Progression Speed | Years to decades | Months to years - fast if untreated |
Other Types of Arthritis You Should Know
OA and RA aren’t the only players. There are over 100 types of arthritis. A few others show up often enough to matter:
Gout
Gout flares up suddenly - often in the big toe. It’s caused by uric acid crystals building up in the joint. The pain is intense, red, and hot. It comes in waves. One day you’re fine, the next you can’t put on a shoe. Diet plays a role: red meat, shellfish, and alcohol raise your risk. Treatment involves medications to lower uric acid and ease flare-ups.
Psoriatic Arthritis
If you have psoriasis - that scaly skin condition - you’re at risk. Psoriatic arthritis affects the skin and joints. Fingers can swell up like sausages. Nails might pit or separate. It can also hurt your spine. Unlike RA, it’s often asymmetrical. Treatment overlaps with RA but includes biologics that target skin inflammation too.
Ankylosing Spondylitis
This one targets the spine. It causes chronic back pain and stiffness, especially in the lower back and hips. It often starts in young adults. Over time, the spine can fuse. It’s linked to the HLA-B27 gene. Exercise and anti-inflammatory drugs help. Some biologics can slow progression.
Why Getting the Right Diagnosis Matters
Take the wrong pill for RA, and you’re wasting time. NSAIDs might ease OA pain, but they won’t stop RA from destroying your joints. DMARDs like methotrexate - the backbone of RA treatment - can cause serious side effects if used in someone who doesn’t need them. And if RA goes untreated for months, you could lose hand function, need surgery, or face heart and lung complications.
On the flip side, if you have OA and start taking strong immune drugs thinking it’s RA, you’re exposing yourself to unnecessary risks: infections, liver damage, even cancer. OA doesn’t need that. It needs movement, weight control, and targeted pain relief.
That’s why seeing a rheumatologist matters. General practitioners can miss the signs. A specialist looks at the pattern - not just the pain. They check for symmetry, systemic symptoms, and blood markers. They use ultrasound to spot early inflammation before X-rays show damage.

Treatment Paths: What Actually Works
OA treatment is about protecting what’s left:
- Weight loss - even small drops make a big difference
- Physical therapy - strengthening muscles around the joint reduces pressure
- NSAIDs like ibuprofen - for flare-ups
- corticosteroid injections - short-term relief
- Joint replacement - for severe cases, especially hips and knees
RA treatment is aggressive and early:
- DMARDs - methotrexate is the first-line drug
- Biologics - drugs like adalimumab or etanercept that block specific immune signals
- JAK inhibitors - newer pills like tofacitinib that work inside cells
- Physical therapy - to maintain mobility
- Regular monitoring - blood tests and imaging to track progress
For both, staying active is non-negotiable. Walking, swimming, cycling - low-impact movement keeps joints flexible and muscles strong. Avoiding inactivity is just as important as taking medication.
What’s New in 2025?
Research is moving fast. For OA, scientists are testing blood and imaging biomarkers to catch cartilage breakdown before X-rays show it. Platelet-rich plasma (PRP) injections are being used more often, though evidence is still mixed. For RA, newer biologics are safer and more targeted. Some patients now reach full remission - meaning no symptoms, no joint damage, no medication needed.
Ultrasound is now standard in early RA diagnosis. It picks up inflammation invisible to X-rays. And AI tools are being trained to spot joint changes in scans faster than human eyes.
The message? Arthritis isn’t one disease. It’s a group. And your treatment depends entirely on which one you have.
Can you have both osteoarthritis and rheumatoid arthritis at the same time?
Yes. It’s not rare. Someone in their 60s with decades of knee wear-and-tear (OA) might also develop RA. The symptoms can overlap, making diagnosis tricky. But the treatment approach changes. You’ll need OA management for the worn joint, plus DMARDs for the autoimmune inflammation. A rheumatologist can untangle the two.
Is arthritis hereditary?
Some types are. OA has a genetic link, especially in hand joints. If your mother had severe OA in her fingers, you’re more likely to develop it. RA has stronger genetic ties - particularly the HLA-DRB1 gene. But having the gene doesn’t mean you’ll get it. Environmental triggers like smoking or infection are usually needed to start the process.
Does weather affect arthritis pain?
Many people swear their joints ache when it’s cold or rainy. Studies show a small but real link - changes in barometric pressure can trigger pain signals in already inflamed or damaged joints. It doesn’t make the disease worse, but it can make symptoms feel worse. Staying warm and moving regularly helps.
Can diet cure arthritis?
No diet cures arthritis. But some foods can help manage inflammation. Omega-3s in fatty fish, antioxidants in berries, and fiber-rich whole grains may reduce flare-ups. Avoiding sugar, processed meats, and refined carbs helps too - especially for RA. For gout, cutting alcohol and red meat is essential. Diet supports treatment - it doesn’t replace it.
When should you see a doctor about joint pain?
See a doctor if pain lasts more than a few weeks, wakes you up at night, or comes with swelling, redness, or fever. If both sides of your body are affected - like both wrists - or you feel unusually tired, don’t wait. Early RA can cause permanent damage in months. OA can be managed better if caught before joints become severely worn.
What to Do Next
If you’re experiencing persistent joint pain, start with your GP. But if symptoms suggest RA - symmetrical swelling, morning stiffness over an hour, fatigue - ask for a referral to a rheumatologist. Don’t settle for "it’s just aging." You deserve to know exactly what’s happening.
Keep a symptom journal: note which joints hurt, how long stiffness lasts, what makes it better or worse. Bring it to your appointment. That simple step helps doctors spot patterns faster.
And remember - arthritis isn’t a death sentence. With the right diagnosis and care, many people live full, active lives. The key is knowing which type you have - and acting fast if it’s rheumatoid.