Why Your Heart Medication Might Be Cheaper Than You Think
If you’re taking more than one pill for your heart every day, you’re not alone. Millions of people in the U.S. are on multiple medications for high blood pressure, cholesterol, or after a heart attack. But here’s the thing: you might not need to take four separate pills. There’s a simpler, cheaper option already out there - cardiovascular combination generics.
These are pills that combine two or more heart medications into one tablet. Think of them as a single pill doing the work of two or three. They’re not new. But they’re still underused. And if you’re paying full price for brand-name combos when generics exist, you’re leaving money on the table - and possibly hurting your health by skipping doses because the regimen is too complicated.
What Exactly Are Cardiovascular Combination Generics?
A cardiovascular combination generic is a single pill that contains two or more generic versions of heart drugs. Common combinations include:
- Statins + ezetimibe (for cholesterol)
- ACE inhibitors + diuretics (for blood pressure)
- Calcium channel blockers + ACE inhibitors
- Aspirin + statin (for post-heart attack care)
These aren’t experimental. The FDA requires generics to match brand-name drugs in strength, safety, and effectiveness. Bioequivalence standards mean the active ingredients must deliver 80-125% of the same amount of drug in your bloodstream as the brand. That’s not a guess - it’s a legal requirement backed by data from over 60 clinical trials reviewed in the European Heart Journal in 2014.
For example, the combo of simvastatin and ezetimibe was once sold as Vytorin. Now, you can buy the generic version for under $10 a month. Same active ingredients. Same results. Same safety profile.
How Much Money Can You Save?
In 2017, Medicare data showed brand-name cardiovascular meds cost an average of $85.43 per prescription fill. Generic combinations? Around $15.67. That’s an 82% drop.
Let’s say you’re on three separate pills: a statin ($30), a blood pressure pill ($25), and aspirin ($5). That’s $60 a month. Switch to a generic combo of statin + blood pressure pill, and you’re down to $18 - plus one less pill to remember.
That’s not just savings. That’s sustainability. People who pay less are more likely to keep taking their meds. And that’s the whole point.
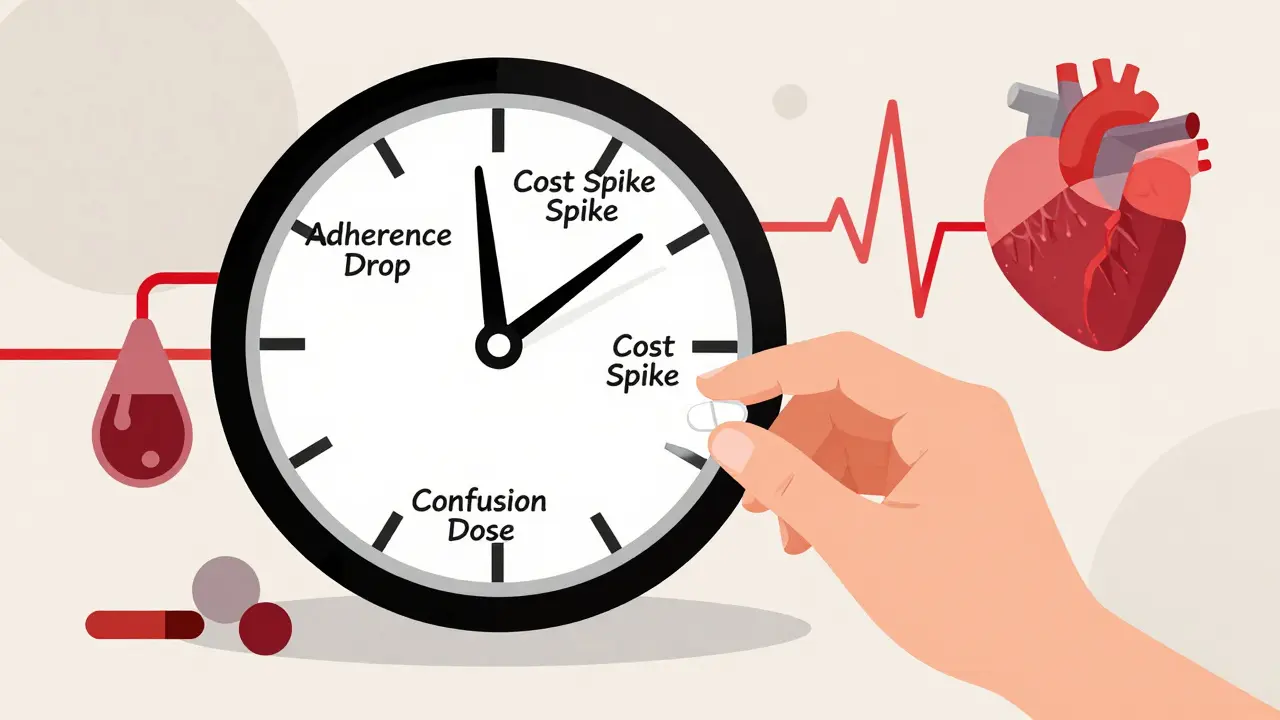
Why Adherence Matters More Than You Realize
Heart disease kills more people than cancer. But here’s the hidden killer: non-adherence. Studies show that when people have to take four or more pills daily, adherence drops to 25-30%. For a single pill, it jumps to 75-85%.
That’s not a small difference. It’s life or death. The American Heart Association calls fixed-dose combinations a Class I recommendation - meaning it’s the strongest possible endorsement for improving outcomes in patients needing multiple drugs.
One 2014 study in the European Heart Journal modeled what would happen if everyone with prior heart disease took a simple “polypill” - aspirin, a statin, an ACE inhibitor, and a beta-blocker in one tablet. The result? A 75% drop in heart attacks and strokes over five years. That’s not theory. That’s data from real-world populations.
And yet, in the U.S., a single pill with all four of those components? Hard to find. In the UK, India, and parts of Latin America, it’s common. In the U.S., you still have to ask for it.
What’s Available Right Now?
Not every combo exists as a generic - but many do. Here’s what’s actually on the market as of 2026:
| Combination | Brand Name (Discontinued) | Generic Availability | Typical Monthly Cost (Generic) |
|---|---|---|---|
| Atorvastatin + amlodipine | Caduet | Yes (since 2016) | $12-$20 |
| Simvastatin + ezetimibe | Vytorin | Yes (since 2016) | $10-$18 |
| Lisinopril + hydrochlorothiazide | Zestoretic | Yes (long available) | $8-$15 |
| Losartan + hydrochlorothiazide | Hyzaar | Yes (since 2012) | $10-$16 |
| Carvedilol + hydrochlorothiazide | Coreg HCT | Yes (since 2017) | $15-$25 |
| Sacubitril + valsartan | Entresto | Yes (since 2022) | $45-$60 |
Notice something? Even the newer, more expensive combos like Entresto (for heart failure) now have generics. That’s huge. What used to cost $600 a month now costs under $60.
What’s Still Missing?
There’s a gap. The ideal “polypill” - aspirin, a statin, an ACE inhibitor, and a beta-blocker - isn’t available as a single pill in the U.S. Why? Regulatory hurdles. Pharma companies don’t invest much in combos if the individual drugs are already cheap. And the FDA doesn’t push for them aggressively.
But you can still get the same effect: ask your doctor for two pills instead of four. For example:
- Pill 1: Atorvastatin (statin)
- Pill 2: Lisinopril + hydrochlorothiazide (blood pressure combo)
- Pill 3: Aspirin 81 mg
That’s three pills. Better than four. And if your doctor prescribes the combo pills where possible, you’re already cutting your pill burden in half.
Are Generics Really as Good as Brand Names?
Yes - but people worry. A 2019 survey by the American Pharmacists Association found 65% of patients feared generics were less effective. The top two concerns? “It won’t work as well” (42%) and “I’ll have side effects” (38%).
Here’s the truth: 78% of patients on Drugs.com rated generic heart meds as “equally effective” as brands. Only 12% reported noticeable side effect changes - and most of those were minor, like a slightly different feeling of fatigue with a generic beta-blocker.
One exception: warfarin. It’s a blood thinner with a narrow window. Even tiny differences in absorption can matter. That’s why many doctors still prescribe brand-name warfarin. But for statins, blood pressure meds, and aspirin? No meaningful difference.
And here’s what pharmacists know: 89% of them routinely explain bioequivalence to patients. They know the data. You should too.
What to Do If Your Doctor Doesn’t Mention Combos
A 2018 study found only 45% of primary care doctors knew all the available generic combinations. That’s not your fault. It’s a system problem.
So here’s what to do:
- Make a list of every pill you take for your heart.
- Check if any can be combined. Use a free tool like GoodRx or your pharmacy’s app to compare prices.
- Ask your doctor: “Are there any generic combo pills that could replace two of these?”
- If they say no, ask: “Why not?”
Don’t be pushy. Be curious. You’re not asking for a miracle. You’re asking for a simpler, cheaper way to stay healthy.
Watch Out for These Pitfalls
Generics aren’t magic. Here’s what can go wrong:
- Switching too fast: If you’re on a brand-name combo and switch to generics, give your body 2-4 weeks to adjust. Don’t panic if you feel slightly different.
- Changing manufacturers: Generic pills from different companies can have different fillers. Rarely, that causes issues. If you notice new side effects after a refill, ask your pharmacist if the maker changed.
- Insurance blocks: Some plans require prior authorization for combos. Call your insurer before switching.
- State laws vary: In 18 states, pharmacists must get your consent before switching a brand to a generic. Know your rights.
What’s Next for Combination Generics?
The future is here - just unevenly distributed. The FDA issued new guidance in 2021 to speed up approval of fixed-dose combos. The World Heart Federation is pushing polypills into low-income countries where heart disease is rising fastest.
Here’s what’s likely to happen in the next 5 years:
- More combos will become generic - especially those with expired patents.
- Insurance plans will push them harder because they save billions.
- Doctors will start prescribing them as first-line, not last-resort.
- Polypills with aspirin + statin + ACE inhibitor + beta-blocker will finally hit U.S. shelves.
For now, the power is in your hands. You don’t need to wait for the system to catch up. Ask for the combo. Save money. Take fewer pills. Live better.
Are cardiovascular combination generics as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet strict bioequivalence standards - meaning they deliver the same amount of active ingredient into your bloodstream as the brand-name version, within a 90% confidence interval. Studies involving over 60 clinical trials, including those reviewed in the European Heart Journal, show no meaningful difference in safety or effectiveness for statins, blood pressure meds, and aspirin combinations. The only exception is warfarin, which requires careful monitoring due to its narrow therapeutic window.
Can I switch from brand-name combo pills to generics on my own?
No. Never switch without talking to your doctor. Even though generics are equivalent, your body may respond differently to new formulations. Your doctor needs to confirm the switch is appropriate for your condition and monitor you for any changes in blood pressure, cholesterol, or side effects. Also, some states require patient consent before a pharmacist substitutes a brand for a generic.
Why aren’t all heart meds available as combination generics?
It’s mostly about business, not science. Once a drug’s patent expires, generic makers focus on single ingredients because they’re cheaper and easier to produce. Combining multiple drugs requires additional testing, regulatory approval, and marketing - which isn’t profitable unless demand is high. Also, some combinations (like aspirin + statin + ACE inhibitor + beta-blocker) haven’t been developed as single pills in the U.S. because no company has pushed for it. That’s changing, but slowly.
How do I know if my pharmacy is giving me the right generic?
Check the label. The name of the manufacturer and the pill’s imprint code (letters/numbers on the tablet) should match what your doctor prescribed. If you get a refill and the pill looks different, ask your pharmacist if the maker changed. Minor differences in shape or color are normal between manufacturers, but if you notice new side effects, report them. Your pharmacist can also tell you if the generic is bioequivalent to the brand.
Do insurance plans cover combination generics?
Yes - and they often prefer them. Most insurance plans, including Medicare Part D, put combination generics on the lowest cost tier. They save insurers money, so they encourage their use. However, some plans require prior authorization for newer combos like sacubitril/valsartan generics. Always check your plan’s formulary or call your insurer before switching.
What if I can’t afford even the generic combo?
Many pharmacies offer $4 generic lists. At Walmart, Target, or Costco, common heart combos like lisinopril/hydrochlorothiazide or atorvastatin/amlodipine can cost under $10 for a 30-day supply. You can also use free apps like GoodRx or SingleCare to compare prices across pharmacies. If you’re on Medicare, ask about Extra Help - a program that lowers prescription costs for low-income patients. No one should skip heart meds because they can’t afford them.
Final Thought: Take One Less Pill
You don’t need to be a doctor to understand this: fewer pills = more adherence = better outcomes. Cardiovascular combination generics aren’t a gimmick. They’re a proven, practical tool - and they’ve been around long enough to be trusted.
Right now, you’re probably paying too much and taking too many pills. You don’t have to accept that. Ask. Compare. Switch. Your heart will thank you.