Imagine you’re a doctor. Your patient walks in with high blood pressure. You reach for your tablet to write a prescription. You pick the most effective drug based on guidelines, clinical history, and side effect profiles. But you don’t know if that pill costs $4 or $400. And you won’t know until the pharmacy calls - or worse, until the patient skips their dose because they can’t afford it.
This isn’t hypothetical. It’s happening every day in clinics across the U.S. And it’s not just about patients struggling to pay. It’s about clinicians - the very people trained to make life-or-death decisions - operating in the dark when it comes to the actual price of the medications they prescribe.
Doctors Are Terrible at Guessing Drug Prices
Studies show doctors are wildly inaccurate when estimating drug costs. One 2007 review of 29 studies found physicians overestimated the cost of cheap generic drugs by 31% and underestimated expensive brand-name drugs by 74%. That’s not a small error. It’s a systemic blind spot.
Why does this matter? Because when you don’t know the price, you can’t choose wisely. A $200 monthly medication might be clinically superior to a $15 generic - but only if the patient can actually afford it. And if you don’t know the difference, you’re prescribing based on theory, not reality.
A 2016 study of 254 medical students and doctors revealed that only 5.4% of generic drug costs and 13.7% of brand-name drug costs were estimated within 25% of the actual price. For most medications, clinicians had no idea. And here’s the kicker: they were more likely to overestimate low-cost drugs than to underestimate expensive ones. That means they’re often choosing pricier options unnecessarily - not because they’re wasteful, but because they’re misinformed.
The System Is Designed to Keep Clinicians in the Dark
Drug pricing in the U.S. is a labyrinth. The same drug can cost $15 at one pharmacy and $320 at another, depending on the patient’s insurance, pharmacy network, and whether they’re paying cash. Manufacturers set list prices. Pharmacies negotiate rebates. Insurers tweak formularies. Patients get stuck with copays that have nothing to do with the drug’s actual cost.
Doctors aren’t trained to navigate this mess. In fact, 56% of U.S. medical schools don’t teach drug pricing at all. Residents learn about pharmacokinetics and drug interactions - but rarely about out-of-pocket costs or insurance formularies. And when they do try to find out, they’re met with broken systems.
One primary care physician on Reddit described spending 3 to 5 minutes per prescription just checking costs - adding over 30 minutes to an already packed clinic day. That’s not efficiency. That’s burnout fuel.
Electronic Health Records Could Fix This - But Most Don’t
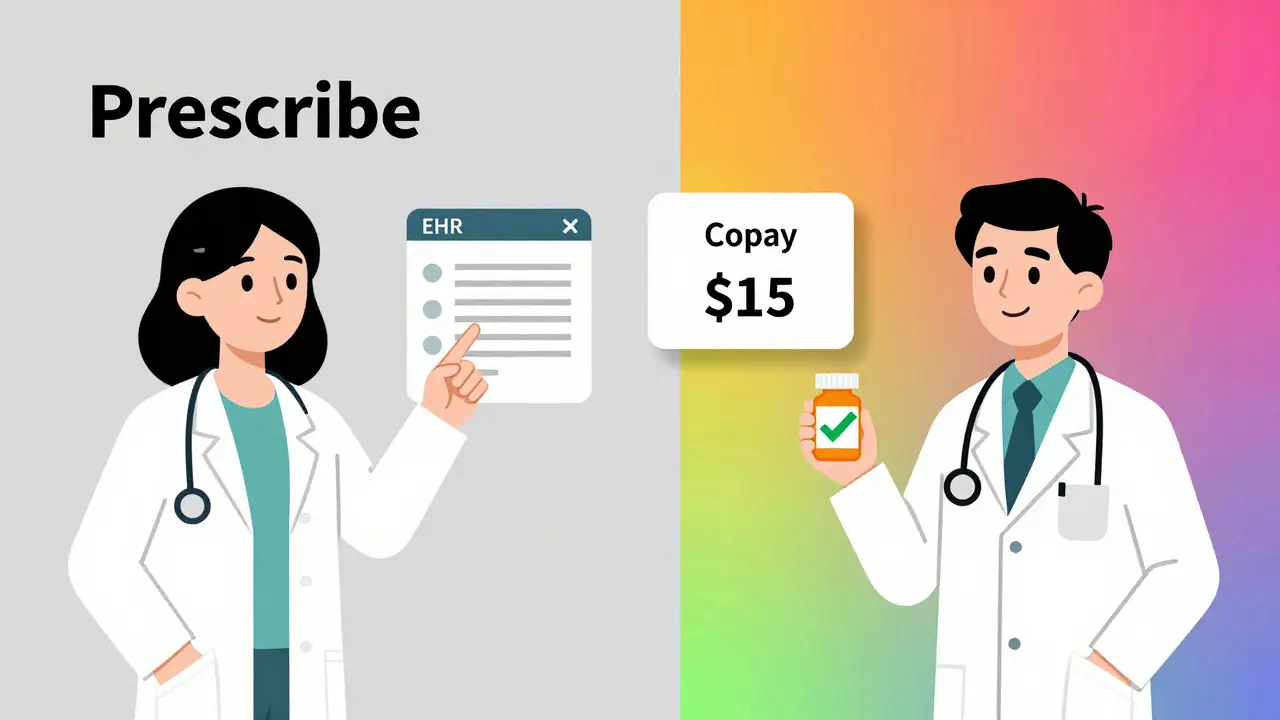
The solution isn’t more training. It’s better tools. Enter EHR cost alerts.
When electronic health records (EHRs) display real-time out-of-pocket costs at the point of prescribing, things change. A 2021 JAMA Network Open study found physicians with access to cost data performed significantly better on cost estimation tasks. But more importantly, they changed their prescribing habits.
In one study, one in eight primary care doctors switched to a cheaper alternative after seeing a cost alert. That number jumped to one in six when the potential savings exceeded $20. That’s not a small impact. That’s hundreds of thousands of prescriptions saved annually - and patients who actually fill their meds.
UCHealth rolled out a real-time benefit tool (RTBT) in 2022. Within months, 12.5% of prescriptions were modified based on cost alerts. But here’s the problem: many of these tools only show insurer-specific prices - not the patient’s actual copay. One internal medicine resident on Reddit complained, “The alert says $80, but my patient’s copay is $150 because their deductible hasn’t been met.” That’s not helpful. That’s misleading.
Who’s Getting It Right?
Some institutions are ahead of the curve. Mayo Clinic’s Drug Cost Resource Guide, updated quarterly since 2019, is rated 4.7 out of 5 by over 1,200 physicians. It’s simple: a searchable database with actual cash prices, insurance tiers, and generic alternatives. No guesswork.
Meanwhile, Medicare’s Part D formulary guide? Rated 2.8 out of 5. Why? Because it’s outdated, cluttered, and doesn’t reflect real-world pricing.
Even better? The new wave of RTBTs are starting to integrate patient-specific factors - like deductible status, prior authorization requirements, and pharmacy network discounts. UCHealth and Harvard are now studying whether these tools reduce disparities. Early data shows safety-net clinics - where patients are more likely to be low-income - see 22% higher prescription modification rates than private practices. That’s not just cost savings. That’s equity.
Doctors Aren’t the Problem - The System Is
Some argue clinicians shouldn’t be burdened with pricing decisions. That’s the job of administrators or pharmacists, they say. But here’s the truth: if you’re the one writing the prescription, you’re the one who holds the power to change it. And if you don’t know the cost, you’re not practicing evidence-based medicine - you’re practicing guesswork.
The American Medical Association and American College of Physicians have both declared cost-conscious prescribing a professional priority since 2015. That’s not a suggestion. It’s a standard. And yet, only 37% of U.S. health systems have implemented any kind of real-time cost tool.
Why? Because it’s expensive. UCHealth spent $2.3 million and 18 months building their system. Many hospitals can’t afford that. Others are waiting for federal mandates.
Change Is Coming - But Not Fast Enough
The 2022 Inflation Reduction Act gave Medicare the power to negotiate prices for 10 high-cost drugs - and more will follow. It’s historic. And it’s popular: 83% of Democrats and 76% of Republicans support it, according to KFF polling.
Meanwhile, CMS now requires drug manufacturers to report out-of-pocket cost estimates. That’s a big step toward transparency. But it doesn’t fix the core issue: clinicians still don’t have this data at their fingertips during the visit.
And the problem keeps growing. In 2023, five major drugs - including Humira - saw price hikes with no clinical justification. The Institute for Clinical and Economic Review found these increases were purely financial. That’s not innovation. That’s exploitation. And clinicians are still flying blind.
What Needs to Happen
Here’s what’s needed - right now:
- Real-time cost data built into every EHR, showing patient-specific copays, not just list prices.
- Training in medical school that includes drug pricing, insurance mechanics, and value-based prescribing.
- Standardized pricing data from manufacturers and insurers - no more 15 different prices for the same pill.
- Financial incentives for hospitals that reduce patient out-of-pocket costs.
Doctors under 40 are adopting these tools at twice the rate of those over 55. That’s not because younger doctors are better. It’s because they grew up with digital tools. They expect information to be available - and they won’t wait for the system to catch up.
The data is clear: when clinicians know the cost, they prescribe better. Patients take their meds. Costs drop. Outcomes improve. And the $187 annual savings per patient? That adds up to billions across the system.
This isn’t about cutting corners. It’s about cutting waste. It’s about making sure the right drug gets to the right patient - without them having to choose between medicine and rent.
It’s time for every clinic, every hospital, every EHR vendor to stop pretending this isn’t their problem. Because it is.
Why don’t doctors know how much drugs cost?
Doctors aren’t trained to track drug prices, and the U.S. healthcare system makes it nearly impossible to get accurate, real-time pricing. Drug costs vary wildly by pharmacy, insurance plan, and patient deductible - and most electronic health records don’t show this information at the point of care. Even when they do, the data is often outdated or incomplete.
Do cost alerts in EHRs actually change prescribing?
Yes. Studies show that when clinicians see real-time out-of-pocket costs during prescribing, one in eight to one in six change their prescription - especially when savings exceed $20 per month. These changes lead to higher medication adherence and lower patient costs without compromising clinical outcomes.
Are generic drugs always cheaper than brand-name drugs?
Not always. While generics are usually cheaper, insurance formularies and pharmacy benefit managers sometimes make brand-name drugs cheaper for patients due to rebates or coupons. In rare cases, a brand-name drug might have a $5 copay while the generic costs $45 because it’s not on the formulary. That’s why real-time, patient-specific data is essential.
How do drug prices get so high?
Drug prices are set by manufacturers, often with little connection to research and development costs. In 2023, drugs like Humira saw price increases of over 4% with no new clinical benefits. Insurers, pharmacies, and PBMs negotiate rebates behind the scenes, but patients still pay inflated list prices - especially if they’re uninsured or underinsured.
Is this problem unique to the U.S.?
Yes. In countries with single-payer or regulated pricing systems, clinicians generally know the cost of medications because prices are standardized. In the U.S., the lack of price transparency is systemic and unique. Clinicians elsewhere rarely face the same confusion or delays when prescribing.
What can patients do to help?
Patients can ask their doctor: ‘Is there a cheaper alternative?’ or ‘Can you check what my copay will be?’ They can also use free tools like GoodRx or their pharmacy’s price checker before the visit. Bringing this information to the appointment helps doctors make better choices - even without EHR alerts.
What Comes Next
The future of prescribing isn’t just about clinical guidelines. It’s about cost transparency. It’s about tools that work. It’s about training that prepares doctors for the real world - not just the textbook.
By 2027, 75% of U.S. health systems are projected to have advanced real-time benefit tools. That’s progress. But it’s not fast enough. Patients are skipping doses now. Families are choosing between insulin and groceries now. And doctors are still guessing.
Knowledge isn’t power - it’s responsibility. And until every clinician has the price in front of them before they hit ‘send,’ we’re not just failing patients. We’re failing the promise of medicine itself.
