Statin Interaction Checker
Check Your Statin Safety
This tool helps identify potentially dangerous interactions between your statin and other medications, supplements, or foods. Results are based on medical guidelines.
Results
Please select options above to see results.
When you’re on a statin, it’s not just about lowering cholesterol. It’s about staying safe while doing it. Many people don’t realize that the statin they’re taking could interact dangerously with other common medications - even over-the-counter ones. The difference between a safe dose and a dangerous one often comes down to which statin you’re on. Not all statins are the same. Some are like firecrackers around certain drugs. Others? They barely blink.
Why Some Statins Are Riskier Than Others
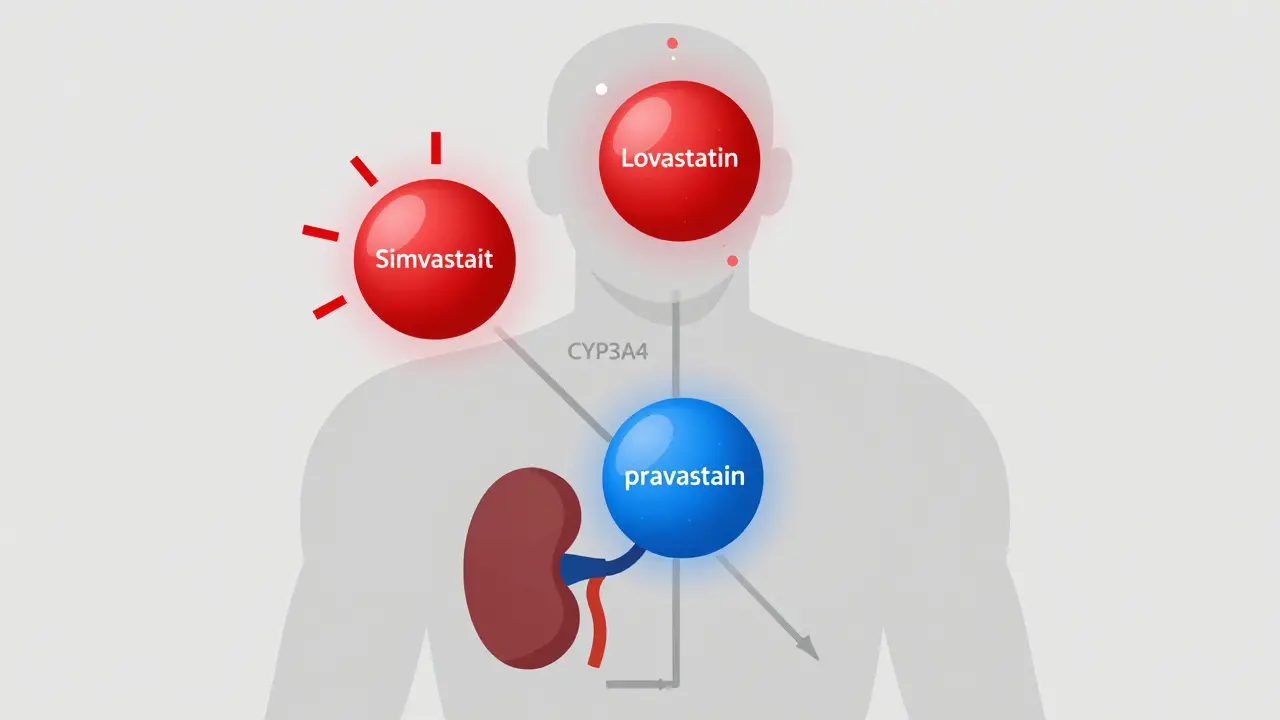
Statins work by blocking an enzyme your liver uses to make cholesterol. But your body doesn’t handle them the same way. Five of the seven statins on the market - simvastatin, lovastatin, atorvastatin, fluvastatin, and the now-withdrawn cerivastatin - rely on liver enzymes called CYP450 to break them down. That’s where the trouble starts.
Simvastatin and lovastatin are the most vulnerable. They’re processed almost entirely by CYP3A4. If you take a drug that blocks this enzyme - like the antibiotic clarithromycin, the antifungal ketoconazole, or even some HIV meds like ritonavir - your body can’t clear the statin fast enough. The result? Statin levels in your blood can spike 10 to 16 times higher than normal. That’s not a typo. That’s enough to cause muscle damage, kidney failure, or even rhabdomyolysis - a rare but life-threatening condition where muscle tissue breaks down and floods your bloodstream.
Atorvastatin is also metabolized by CYP3A4, but it’s a bit more forgiving. With clarithromycin, its levels only rise about fourfold. Still, that’s enough to warrant caution. Fluvastatin uses a different enzyme - CYP2C9 - so it avoids many of the common CYP3A4 interactions. But it’s not safe from everything. If you’re on warfarin or certain diabetes drugs, watch out.
The Quiet Players: Pravastatin, Rosuvastatin, and Pitavastatin
Then there are the quiet ones: pravastatin, rosuvastatin, and pitavastatin. They barely touch CYP enzymes. Pravastatin is mostly cleared by the kidneys. Rosuvastatin and pitavastatin get broken down by glucuronidation - a different pathway entirely. That makes them safer choices if you’re on multiple medications.
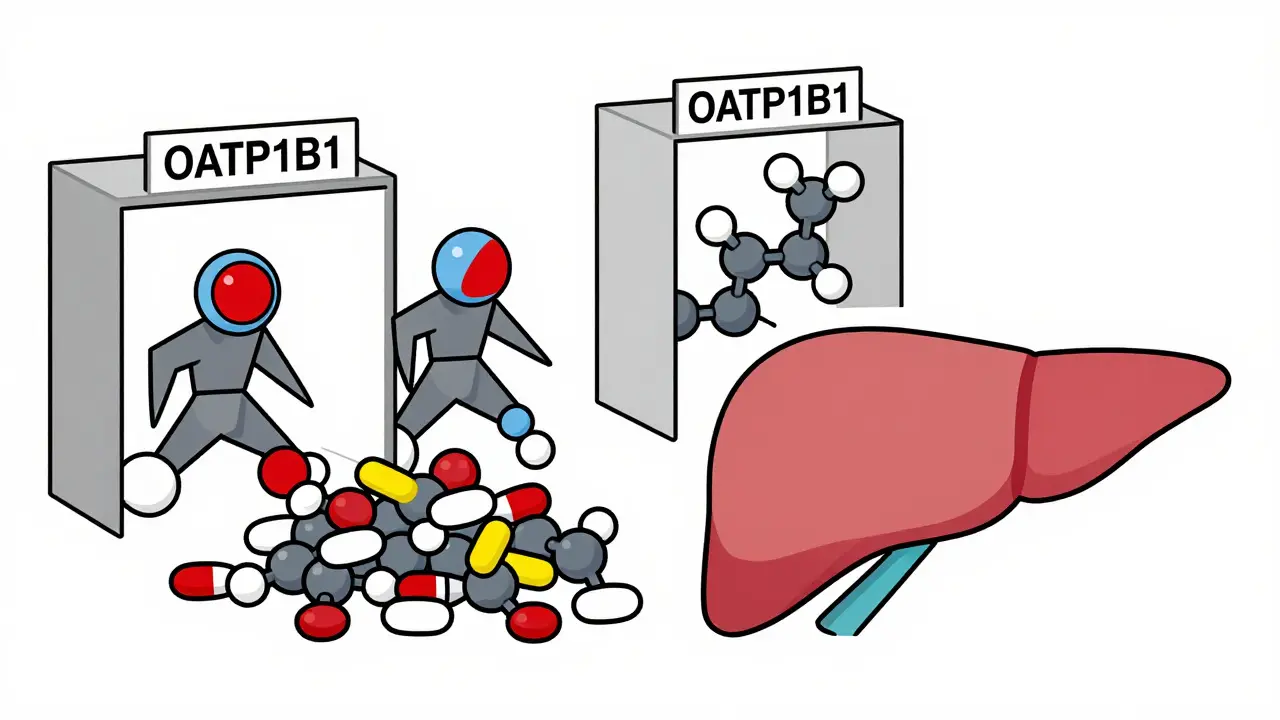
But here’s the catch: even these statins have their own trap. They all rely heavily on a transporter called OATP1B1 to get into your liver. If something blocks that transporter - like cyclosporine (used after organ transplants) or gemfibrozil (a fibrate for triglycerides) - the statin can’t enter your liver properly. Instead, it builds up in your blood. Cyclosporine can boost rosuvastatin levels by nearly sevenfold and pitavastatin by the same amount. That’s why the FDA says: never combine cyclosporine with lovastatin, simvastatin, or pitavastatin. Pravastatin is the only one allowed with cyclosporine, up to 40 mg per day.
Pravastatin stands out as the safest overall. It’s hydrophilic (water-soluble), so it doesn’t cross into muscle tissue easily. That means less risk of muscle pain or damage. It’s also the only statin that doesn’t need dose adjustment with most common drugs. If you’re on a complex med list - say, blood pressure pills, antifungals, or even some antidepressants - pravastatin is often the go-to.
What About Fibrates and Colchicine?
Many people with high cholesterol also have high triglycerides. That’s where fibrates come in. But combining them with statins is risky. Gemfibrozil is the worst offender. It blocks not just CYP2C8, but also glucuronidation - the backup pathway for rosuvastatin and pitavastatin. Studies show it can double statin levels in the blood. The American Heart Association says: avoid gemfibrozil with all statins except pravastatin.
Fenofibrate is a better alternative. It doesn’t interfere with statin metabolism the same way. If you need a fibrate, choose fenofibrate. It’s safer, and studies show it doesn’t increase muscle damage risk the way gemfibrozil does.
Colchicine - used for gout flares - is another silent risk. It doesn’t block CYP enzymes, but it can still raise the chance of muscle toxicity when paired with statins. The advice? You don’t need to stop the statin. But your doctor should lower the dose and watch you closely. Especially if you’re over 70, have kidney issues, or are on multiple meds.
Heart Drugs That Clash With Statins
Ticagrelor (Brilinta) is a blood thinner used after heart attacks. It’s commonly prescribed with statins. But here’s what you need to know: ticagrelor slightly increases the levels of simvastatin and lovastatin. That’s why the American College of Cardiology says: never give simvastatin or lovastatin above 40 mg daily if you’re also on ticagrelor. Atorvastatin? It’s fine. The interaction is minimal. No dose change needed.
Calcium channel blockers like diltiazem and verapamil - used for high blood pressure and angina - are another concern. They block CYP3A4. When taken with simvastatin or lovastatin, they can triple or even quadruple statin levels. That’s why doctors often switch patients on these blood pressure meds to pravastatin or rosuvastatin. Atorvastatin can still be used, but only at lower doses and with monitoring.
Genetics Matter More Than You Think
Two people can take the exact same dose of simvastatin, with the same other meds, and one gets muscle pain while the other feels fine. Why? Genetics.
The SLCO1B1 gene controls the OATP1B1 transporter. About 15% of people have a variant called c.521T>C. If you have it, your body can’t move simvastatin into your liver efficiently. That means more statin floating around in your blood - and a 4.5 times higher risk of muscle damage. The FDA added this genetic warning to simvastatin labels back in 2011. It’s not routine testing yet, but if you’ve had unexplained muscle pain on statins, ask your doctor about it.
That same gene variant also affects rosuvastatin and pitavastatin, but less dramatically. Pravastatin? It’s not affected at all. That’s another reason it’s the safest for people with complex genetics or family histories of statin intolerance.
What Should You Do?
If you’re on a statin and take other meds - even aspirin, herbal supplements, or OTC painkillers - talk to your pharmacist or doctor. Don’t assume it’s safe. Many interactions are silent until it’s too late.
Here’s a simple checklist:
- Ask: Which statin am I on? Write it down.
- Make a list of every medication, including vitamins and supplements.
- Check if you’re on cyclosporine, clarithromycin, gemfibrozil, or HIV meds. If yes, your statin may need to change.
- Ask if you’ve ever had unexplained muscle pain, weakness, or dark urine. That’s a red flag.
- If you’re over 65, have kidney disease, or take multiple drugs, pravastatin or rosuvastatin are often the best choices.
Don’t stop your statin on your own. The benefits of lowering LDL cholesterol - preventing heart attacks, strokes, and death - still outweigh the risks for most people. But you need to manage those risks smartly.
What’s Next?
Researchers are working on tools that use your DNA to predict which statin you’ll tolerate best. The NIH is funding a project to build a clinical decision system that combines your genetics, current meds, and liver function to recommend the safest statin - in real time.
Meanwhile, newer drugs like bempedoic acid (Nexletol) are coming onto the market. It lowers cholesterol without relying on liver enzymes. No CYP interactions. No OATP1B1 issues. It’s not a statin, but for people who can’t tolerate them, it’s a real alternative.
Bottom line: your statin isn’t just a pill. It’s part of a system. And that system can break if you don’t know how it works. The right statin for you isn’t the cheapest one. It’s the one that won’t hurt you when you take it with everything else you’re on.
Can I take grapefruit juice with my statin?
Grapefruit juice blocks CYP3A4, so it can dangerously raise levels of simvastatin, lovastatin, and atorvastatin. Even one glass can cause problems. Avoid it completely if you’re on any of those. Pravastatin, rosuvastatin, and pitavastatin are safe with grapefruit juice.
Is one statin better for the liver than another?
All statins can cause mild liver enzyme increases, but that’s usually harmless. Pravastatin and rosuvastatin are least likely to affect the liver because they’re not heavily metabolized by liver enzymes. If you have existing liver disease, these are often preferred. But if liver enzymes rise more than three times the normal level, your doctor will likely stop the statin - no matter which one you’re on.
Why is simvastatin 80 mg no longer recommended?
The FDA pulled the 80 mg dose of simvastatin in 2011 because studies showed it increased the risk of muscle damage without giving extra heart protection. Even at lower doses, it’s risky if you’re on other meds. Today, 40 mg is the max, and only if you’ve been on it for a year without problems.
Can I switch statins if I have side effects?
Yes. If you have muscle pain or other side effects, switching to a different statin often helps. Pravastatin and rosuvastatin are the most common switches because they’re less likely to cause problems. Don’t give up on statins - just find the right one for your body.
Do I need blood tests while on statins?
Yes. Your doctor should check your liver enzymes and creatine kinase (CK) before you start, and again after 3-6 months. If you develop muscle pain, weakness, or dark urine, get tested immediately. These tests catch problems early - before they become serious.
Final Thought
Statins save lives. But they’re not one-size-fits-all. The difference between safety and danger often comes down to the name on the bottle. Know which one you’re on. Know what you’re taking with it. And never assume it’s fine just because your doctor prescribed it. Your life depends on the details.