Elderly Renal Dosing Calculator
Why This Matters
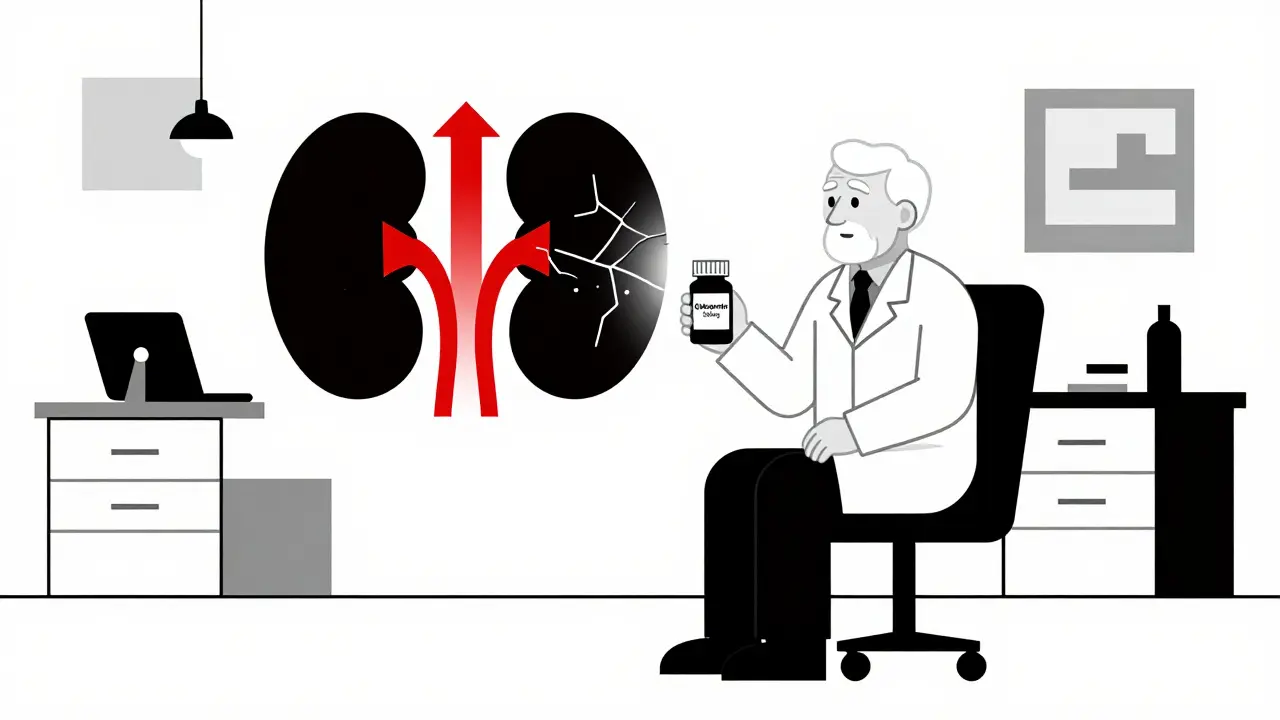
Kidney function declines 1% per year after age 40. Using standard doses in elderly patients with renal impairment can lead to toxicity, falls, confusion, and hospitalization. This tool helps adjust doses based on accurate kidney function assessment.
When you’re over 65 and your kidneys aren’t working like they used to, taking the same pills you did at 50 can be dangerous. It’s not about being old-it’s about how your body changes. Your kidneys filter drugs out of your blood. When they slow down, those drugs build up. And in older adults, even a small buildup can cause falls, confusion, hospital stays, or worse. This isn’t rare. About 38% of adults 65 and older have moderate to severe kidney impairment. Yet, many doctors still prescribe standard doses. That’s why knowing how to adjust medication for elderly renal impairment isn’t just helpful-it’s life-saving.
Why Kidney Function Matters More After 65
Your kidneys don’t just make urine. They clean your blood. Every pill you take-antibiotics, painkillers, blood pressure meds-passes through them. As you age, kidney function naturally declines. Glomerular filtration rate (GFR), the gold standard for measuring kidney health, drops by about 1% per year after age 40. By 70, many people have a GFR below 60 mL/min/1.73 m²-the threshold for chronic kidney disease. But here’s the catch: many older adults don’t know their GFR. Their doctors don’t test it. And if they do, they often rely on outdated methods that give the wrong number.That’s a problem because most drugs are cleared by the kidneys. If your kidneys are at 40% capacity but you’re still taking a full dose, you’re essentially giving yourself 2.5 times the intended amount. For drugs with a narrow safety window-like digoxin, lithium, or vancomycin-that’s a recipe for toxicity. Digoxin levels above 2.0 ng/mL can cause fatal heart rhythms. Lithium above 1.2 mmol/L can lead to seizures. These aren’t theoretical risks. They happen every day in nursing homes and ERs.
How to Measure Kidney Function Accurately
You can’t guess kidney function. You have to measure it. But not all tests are equal. The most common method is the Cockcroft-Gault equation, which uses age, weight, sex, and serum creatinine. It’s old-developed in 1976-but still the most reliable for dosing in older adults. Why? Because newer equations like MDRD or eGFR, which are widely used in labs, tend to overestimate kidney function in elderly patients by 15-20%. That means if your eGFR says you’re at 45 mL/min, your real kidney function might be closer to 35. That difference could mean the difference between a safe dose and a toxic one.For people over 70, or those with low muscle mass (common in frail elderly), creatinine-based tests are especially misleading. Creatinine comes from muscle. Older people lose muscle. So even if their creatinine looks normal, their kidneys may be failing. That’s why some experts now recommend adding cystatin C, a protein less affected by muscle mass, to get a clearer picture. But cystatin C isn’t available everywhere. In community clinics, you’re likely stuck with creatinine. So use Cockcroft-Gault. Always. And never trust a lab’s eGFR number without checking the calculation.
Which Medications Are Most Dangerous?
Not all drugs are created equal. Some are safe even with poor kidney function. Others are ticking time bombs. Here’s what to watch for:- Metformin: Used for diabetes, it’s one of the most common culprits. In the U.S., guidelines say to stop it if creatinine is above 1.5 mg/dL in men or 1.4 mg/dL in women. But European guidelines are more flexible-monitoring is enough. The key is knowing your patient’s history. If they’ve had heart failure or dehydration, stop it.
- Gabapentin: Used for nerve pain and seizures. It’s eliminated almost entirely by the kidneys. Standard dose? 300-1200 mg daily. For GFR below 30? Cut it to 100-300 mg daily. Yet studies show 68% of prescribers get this wrong. The result? Dizziness, falls, broken hips.
- Rivaroxaban: A blood thinner. If kidney function drops below 30 mL/min, the risk of bleeding skyrockets. Many doctors still prescribe the full dose. That’s why 52% of dosing errors involve this drug.
- Allopurinol: For gout. The standard dose is 300 mg daily. For GFR under 10? Start with 100 mg every other day. Too much causes a deadly skin reaction called Stevens-Johnson syndrome.
- Cefepime: An antibiotic. For GFR 30-50? Give it every 8 hours instead of every 6. For GFR under 10? Only once a day. Too frequent? Seizures.
Some drugs are safer than you think. Glipizide, a diabetes pill, doesn’t need dose adjustment. Ibuprofen? Avoid it altogether-worse for kidneys than most people realize. Always check the drug’s renal clearance percentage. If it’s over 50%, assume it needs adjustment.

The 50% Rule-And Why It Fails
Many doctors use a shortcut: if kidney function is below 50 mL/min, cut the dose in half. It’s simple. And it’s wrong. A 2011 KDIGO report found this rule fails for 22% of high-risk medications. Why? Because not all drugs behave the same. Vancomycin, for example, has nonlinear pharmacokinetics. Halving the dose doesn’t halve the blood level-it can make it unpredictable. For drugs like this, you need to extend the interval, not reduce the dose. Vancomycin might go from every 12 hours to every 48 hours, keeping the same dose but giving the kidneys more time to clear it.Another mistake: using ideal body weight instead of actual weight. If a patient is overweight, using their ideal weight can lead to underdosing. For obese patients, use adjusted body weight. For frail patients, use actual weight. Context matters. No one-size-fits-all.
How to Get It Right: Tools and Systems That Work
The biggest problem isn’t knowledge-it’s execution. A 2015 study found only 44% of prescribers consistently adjusted doses. Why? Busy clinics. Outdated charts. No alerts. The solution isn’t more training-it’s better systems.Electronic health records (EHRs) can help. The University of Nebraska Medical Center added automated alerts that pop up when a doctor orders a drug like gabapentin or rivaroxaban for a patient with low GFR. Within a year, dosing errors dropped by 37%. That’s real impact.
Pharmacist-led programs are even better. At Mayo Clinic, clinical pharmacists reviewed all medications for patients over 65 with kidney disease. Result? A 58% drop in adverse drug events. Pharmacists catch what doctors miss: drug interactions, hidden metabolites, outdated guidelines.
There are apps too. Epocrates Renal Dosing, used over 1.2 million times, gives instant dose adjustments for 150+ drugs. But don’t rely on apps alone. Use them with lab values and clinical judgment.

What’s New in 2026
The field is changing fast. In early 2023, the FDA approved the first AI-powered dosing tool, DoseOptima. It pulls real-time lab data, age, weight, and medication list, then recommends exact doses. In a trial of 15,000 patients, it was 92.4% accurate. It’s not everywhere yet-but it’s coming.KDIGO’s new guidelines, expected late 2023, will make cystatin C the preferred test for elderly patients. That’s a big shift. And the American Society of Health-System Pharmacists is finalizing a national standard for dosing 150 high-risk drugs. By 2026, hospitals that don’t use these standards will be outliers.
Even insurance is pushing change. Medicare penalizes hospitals with high rates of adverse drug events. That means institutions now have financial reasons to get dosing right. In 2022, one hospital lost $17,000 per bed annually for poor performance. That’s not a small penalty.
What You Can Do Today
If you’re caring for an older adult:- Ask for their serum creatinine and GFR. Don’t assume it’s normal.
- Use the Cockcroft-Gault equation. Plug in their age, weight, sex, and creatinine. Don’t trust the lab’s eGFR without checking.
- Check every medication. Is it cleared by the kidneys? Is it on the Beers Criteria list? Is there a safer alternative?
- Start low, go slow. Especially with pain meds, antibiotics, and diabetes drugs.
- Ask for a pharmacist consult. Most hospitals have them. Ask your doctor to involve one.
Don’t wait for a crisis. A single dose error can lead to a hospital stay that changes everything. And if you’re a clinician: if you’re not checking kidney function before prescribing, you’re gambling. With someone’s life.
When to Worry: Red Flags in Elderly Patients
Look for these signs after a new medication is started:- Sudden confusion or memory loss
- Unexplained dizziness or falls
- Loss of appetite, nausea, vomiting
- Swelling in legs or ankles
- Changes in urination-too much or too little
- Irregular heartbeat
These aren’t just ‘old age.’ They’re signs of drug toxicity. Stop the drug. Check kidney function. Call a pharmacist. Don’t wait.
What’s the most common mistake doctors make with elderly renal impairment?
The biggest mistake is assuming that a normal serum creatinine means normal kidney function. In older adults, low muscle mass means creatinine stays low even when kidneys are failing. Many doctors rely on lab eGFR numbers without checking if they were calculated with Cockcroft-Gault. The result? They give full doses of drugs like gabapentin or rivaroxaban, leading to falls, bleeding, or hospitalization.
Can I just reduce all doses by 50% for elderly patients?
No. The 50% rule works for some drugs, like gabapentin or cefdinir, but fails for others. Vancomycin, for example, needs longer dosing intervals, not lower doses. Lithium and digoxin require precise blood level monitoring. Using a blanket reduction can lead to underdosing or overdosing-both are dangerous. Always check drug-specific guidelines.
Is metformin safe for elderly patients with kidney disease?
It depends. U.S. guidelines say to stop metformin if creatinine is above 1.5 mg/dL in men or 1.4 mg/dL in women. But European guidelines allow it with close monitoring if GFR is above 30 mL/min. The key is avoiding dehydration, heart failure, or contrast dye. If the patient is stable and well-hydrated, metformin can be used safely-even with mild kidney impairment. Never assume it’s unsafe without checking the full picture.
How often should kidney function be checked in elderly patients on chronic meds?
At least every 3-6 months for those with known kidney impairment or on high-risk drugs like NSAIDs, diuretics, or antihypertensives. For patients on drugs like digoxin or lithium, check creatinine and drug levels every 3 months. If there’s a change in health-dehydration, infection, hospitalization-check immediately. Kidney function can drop quickly in older adults.
Are there any medications that are always safe in elderly renal impairment?
Few are completely safe, but some require no dose adjustment. Glipizide (a diabetes drug), citalopram (an antidepressant), and oxycodone (a painkiller) are primarily metabolized by the liver, not the kidneys. That makes them safer options. But even these can cause side effects in frail patients. Always start low and monitor closely. No drug is risk-free in older adults.