When you start a GLP-1 medication like Wegovy, Ozempic, or Mounjaro for weight loss, the first thing you’ll hear from your doctor is: nausea is common. It’s not a bug-it’s part of how the drug works. These medications slow down your stomach, so you feel full faster and stay full longer. But that same mechanism can make you feel queasy, especially in the first few weeks. If you’re one of the 30-45% of people who get nauseous, you’re not alone. And you don’t have to quit. Most people get through it-and lose weight-by adjusting how they take it.
Why GLP-1 Medications Cause Nausea
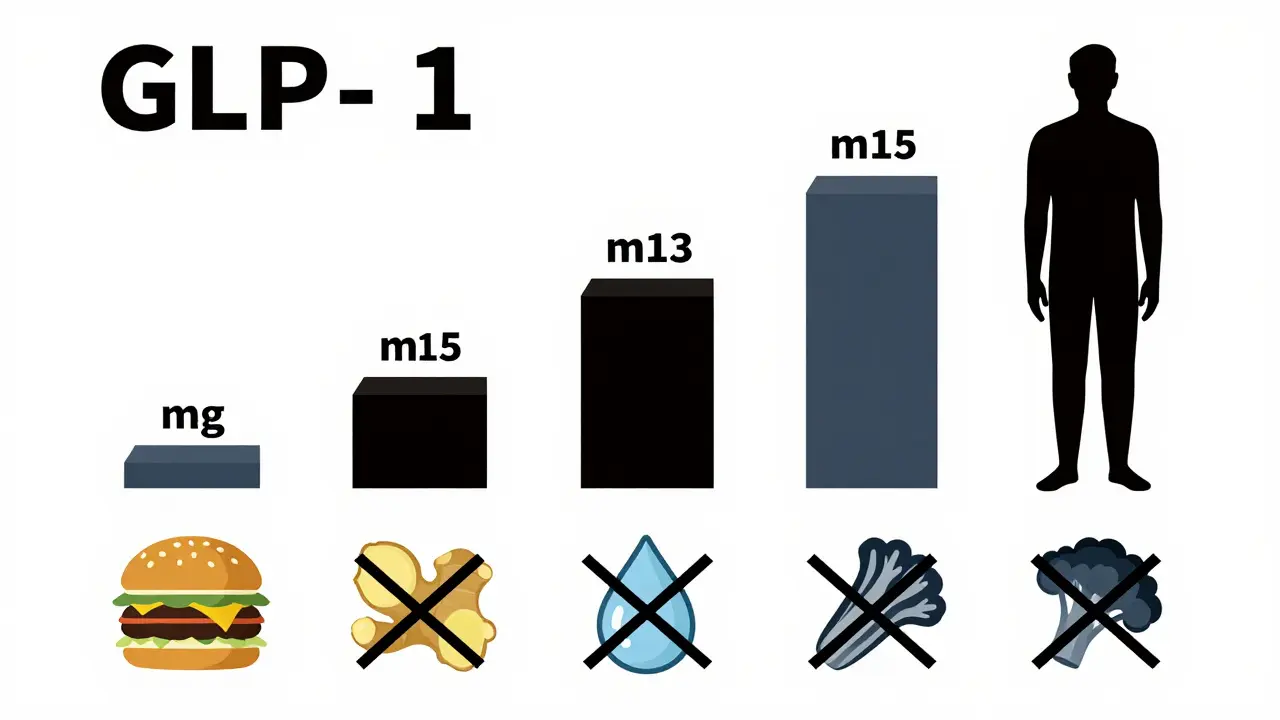
GLP-1 drugs mimic a natural hormone your body makes after eating. That hormone tells your pancreas to release insulin, tells your liver to stop pumping out sugar, and-most importantly-slows how fast your stomach empties. That’s why you don’t feel hungry as often. But it also means food sits in your stomach longer. If you eat too much, too fast, or eat greasy foods, your stomach gets backed up. That’s when nausea hits.It’s not just in your head. Studies show nausea peaks during dose increases. When you go from 0.25 mg to 0.5 mg of semaglutide, your body isn’t ready for the sudden change in stomach speed. The same goes for tirzepatide when you jump from 5 mg to 7.5 mg. The side effect isn’t random-it’s tied directly to the dose.
Dosing Schedules That Reduce Nausea
The key to avoiding severe nausea isn’t avoiding the drug-it’s going slow. Every major GLP-1 medication has a built-in ramp-up schedule for this exact reason.- Wegovy (semaglutide for weight loss): Starts at 0.25 mg once a week for 4 weeks. Then it climbs: 0.5 mg (weeks 5-8), 1 mg (weeks 9-12), 1.7 mg (weeks 13-16), and finally 2.4 mg from week 17. That’s 17 weeks just to reach the full dose.
- Mounjaro (tirzepatide): Begins at 2.5 mg weekly. Increases by 2.5 mg every 4 weeks: 5 mg, 7.5 mg, 10 mg, then 12.5 mg and 15 mg. Total time to max dose: about 20 weeks.
- Ozempic (semaglutide for diabetes): Starts at 0.25 mg, moves to 0.5 mg after 4 weeks, then 1 mg. Max dose is 2 mg.
- Victoza (liraglutide): Begins at 0.6 mg daily, then increases to 1.2 mg or 1.8 mg after a week.
These aren’t suggestions-they’re proven paths. A Cleveland Clinic survey found patients who followed the full titration schedule had 63% less nausea than those who rushed it. Skipping steps or doubling up doses doesn’t speed up weight loss. It just makes you sicker.
What Actually Helps With Nausea
If you’re feeling nauseous, here’s what works-based on patient reports, doctor recommendations, and clinical data:- Take it at bedtime. Over 60% of users report less nausea when they inject before sleep. Your body is resting, digestion slows naturally, and you’re less likely to notice the discomfort.
- Eat smaller, more frequent meals. Instead of three big meals, try five small ones. A slice of turkey, a boiled egg, or a cup of Greek yogurt is easier to handle than a steak dinner.
- Avoid high-fat and fried foods. Fat takes longer to digest. When your stomach is already slowed down, grease is the worst thing you can add. Stick to lean proteins, vegetables, and whole grains.
- Stay hydrated-but not with sugary drinks. Water, herbal tea, or sparkling water help. Avoid soda, juice, or sweetened coffee. Sugar can trigger more nausea and spike blood sugar, which defeats the purpose.
- Try ginger. Ginger tea, ginger chews, or capsules are recommended by 78% of obesity specialists. It’s one of the few natural remedies with real evidence behind it.
- Don’t lie down right after eating. Wait at least 90 minutes. Gravity helps keep food moving.
One Reddit user, @WeightLossWarrior87, wrote: “Week 1 on 0.25 mg was brutal. I threw up twice. Week 3 at 0.5 mg? I ate a salad and didn’t feel a thing.” That’s not luck-it’s timing and tweaks.
When to Pause or Stop
Mild nausea that fades after a week or two? That’s normal. But if you’re vomiting daily, losing weight you can’t afford to lose, or feeling dizzy and dehydrated, it’s time to pause.Dr. David Ludwig from Harvard says: “Persistent nausea isn’t a sign you’re doing it right-it’s a sign you need to adjust.” If nausea lasts longer than 2-3 weeks at a new dose, talk to your provider. You might need to stay at your current dose longer, or temporarily drop back a step. Most clinics now offer telehealth check-ins just for this reason.
Don’t confuse nausea with a reaction to the injection itself. If you have swelling, redness, or pain at the injection site, that’s different. Nausea is internal. Injection site issues are local. If you’re unsure, call your doctor.
What Doesn’t Work
There are a lot of myths floating around. Here’s what to ignore:- “Just push through it.” No. If you’re vomiting, you’re not building tolerance-you’re risking dehydration and electrolyte imbalance.
- “Take an anti-nausea pill like Dramamine.” Over-the-counter meds like this don’t help with GLP-1 nausea. They target motion sickness, not slowed digestion.
- “Switch to compounded versions.” The FDA has warned against these. They’re not tested for safety or purity. Some have been found to contain harmful additives or wrong dosages.
- “Wait until I lose 10 pounds before I worry about nausea.” Weight loss takes time. Most people lose only 2-3% in the first 8 weeks. Nausea doesn’t mean the drug isn’t working-it means your body is adjusting.

Long-Term Outlook: Does Nausea Go Away?
Yes-for most people. A survey by the Obesity Action Coalition found that 89% of patients who stuck with the medication past 12 weeks (even with initial nausea) lost at least 5% of their body weight. And by month 6, 72% reported nausea was either gone or barely noticeable.Why? Your body adapts. The receptors in your gut get used to the medication. Your stomach learns to empty a little faster again. You also learn what foods you can handle. It’s not magic-it’s biology and behavior working together.
Even better: once you’re at your maintenance dose, nausea often drops dramatically. A study in the New England Journal of Medicine showed that while 45% had nausea at the start of the 2.4 mg dose, only 18% still had it after 12 months.
What’s Next for GLP-1 Medications
The future is getting better. In 2025, Novo Nordisk plans to launch an oral version of semaglutide. Early trials suggest it causes 30-40% less nausea than the injectable form. That could change everything for people who hate needles or can’t tolerate side effects.Meanwhile, insurance coverage is slowly improving. In 2023, 32% of Fortune 500 companies started covering GLP-1 drugs for weight loss-up from 9% in 2021. And new data from the SELECT trial showed that semaglutide reduces heart attacks and strokes by 20% in people with obesity-even without diabetes. That’s making doctors more confident prescribing these drugs long-term.
But supply is still tight. Wegovy and Ozempic were on the FDA’s drug shortage list for over a year through late 2023. If you’re on one, don’t skip doses. Talk to your pharmacy early if you’re running low. Some clinics now offer backup prescriptions or temporary alternatives.
Final Thoughts: It’s a Marathon, Not a Sprint
GLP-1 medications aren’t magic pills. They’re powerful tools-and like any tool, they need to be used right. Nausea isn’t a dealbreaker. It’s a signal. Listen to your body. Stick to the dosing schedule. Eat smart. Stay hydrated. And don’t give up in the first month.People who make it through the first 12 weeks don’t just lose weight. They change how they eat. They learn to listen to hunger cues. They start moving more. That’s the real win-not the scale, but the habits you build along the way.
How long does nausea last on GLP-1 medications?
For most people, nausea peaks during the first 2-4 weeks at each new dose and improves within 1-2 weeks after settling into that dose. By the time you reach your maintenance dose (usually around 16-20 weeks), nausea is significantly reduced or gone for 70% of users.
Can I take anti-nausea medicine with GLP-1 drugs?
Over-the-counter drugs like Dramamine or Pepto-Bismol don’t help with GLP-1-induced nausea because they don’t target the root cause-slowed stomach emptying. Prescription anti-nausea meds like ondansetron may help in severe cases, but only under a doctor’s supervision. The best approach is dietary and timing adjustments, not medication.
Should I skip a dose if I’m nauseous?
Don’t skip unless you’re vomiting or dehydrated. Missing one dose won’t hurt your progress, but skipping regularly can stall weight loss and make it harder to resume. If nausea is mild, keep taking it at bedtime with bland food. If it’s severe, contact your provider to pause your dose increase-not the medication entirely.
Do all GLP-1 drugs cause the same level of nausea?
No. Tirzepatide (Mounjaro/Zepbound) tends to cause slightly more nausea than semaglutide (Wegovy/Ozempic) at equivalent weight-loss doses. Liraglutide (Victoza) generally causes the least nausea but also leads to less weight loss on average. The trade-off is effectiveness vs. tolerability.
Is nausea a sign the drug is working?
Not exactly. Nausea happens because the drug slows your stomach-but you can still lose weight without it. Some people experience strong satiety with little to no nausea. The goal isn’t to suffer-it’s to find the dose and routine that gives you results with minimal discomfort.
Can I drink alcohol while on GLP-1 medication?
It’s not recommended, especially early on. Alcohol can irritate your stomach, lower blood sugar, and worsen nausea. If you do drink, wait until you’re at your maintenance dose and stick to small amounts of low-sugar options like dry wine or spirits with soda water. Avoid beer and cocktails with syrup.
What if I can’t afford GLP-1 medications?
Annual costs range from $9,000 to $13,000 without insurance. Some manufacturers offer savings cards-Novo Nordisk has a Wegovy Support Program, and Eli Lilly has Mounjaro Care. Check if your employer covers it-32% of Fortune 500 companies now do. Some clinics offer payment plans or clinical trial options. Never buy from unverified online sellers.
