Women with PCOS often struggle with more than just irregular periods and acne. For many, the real battle is with weight - stubborn, hard-to-lose weight that comes with insulin resistance, high testosterone, and a slow metabolism. Traditional treatments like metformin help, but they rarely deliver the kind of results that change lives. That’s where GLP-1 receptor agonists come in. These aren’t magic pills, but they’re the most effective weight-loss drugs we’ve seen for PCOS in decades.
What Are GLP-1s, Really?
GLP-1s - glucagon-like peptide-1 receptor agonists - were first made to treat type 2 diabetes. But doctors quickly noticed something surprising: patients weren’t just controlling their blood sugar. They were losing weight. A lot of it. Liraglutide (Saxenda) got FDA approval for obesity in 2014. Semaglutide (Wegovy) followed in 2021. Both work by mimicking a natural gut hormone that tells your brain you’re full, slows down digestion, and helps your pancreas release insulin only when needed.
They don’t just reduce hunger. They change how your body stores fat. In women with PCOS, where up to 80% struggle with obesity, this matters. Losing even 5% of body weight can bring back periods, lower testosterone, and improve insulin sensitivity. GLP-1s do that - and then some.
How Much Weight Do You Actually Lose?
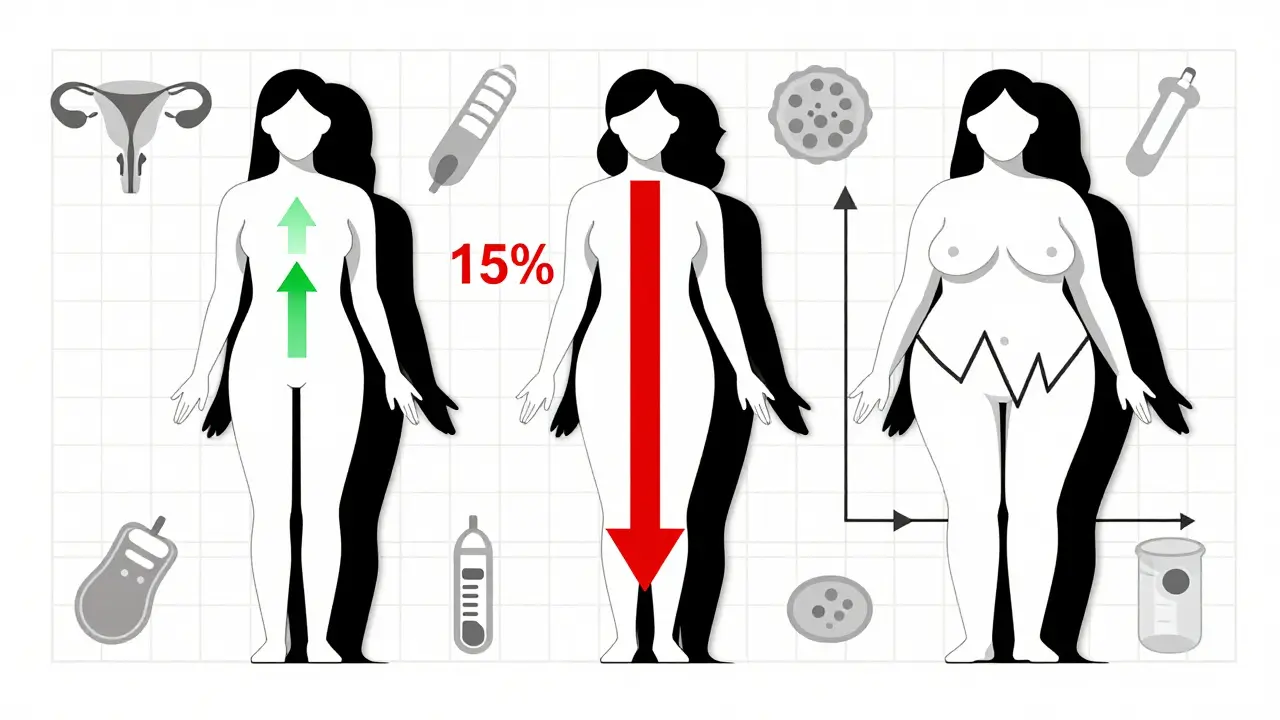
Let’s get specific. In clinical trials, women with PCOS using liraglutide lost about 5-10% of their body weight over six months. Those on semaglutide lost even more - up to 14-15% over a year. One study found that after 68 weeks on semaglutide 2.4 mg, women lost nearly 15% of their starting weight. That’s not just a few pounds. That’s going from a size 16 to a size 10.
Compare that to metformin, the old standard. Metformin typically helps women lose 2-5% of body weight. GLP-1s beat that. In head-to-head studies, semaglutide led to 1.5 kg/m² greater BMI reduction than metformin. Visceral fat - the dangerous kind around your organs - dropped by 18% in PCOS patients using semaglutide. That’s not just cosmetic. That’s lowering your risk of heart disease and diabetes.
It’s Not Just About Weight
Weight loss is the headline, but the real win is what happens underneath. In a 2022 study, 68% of women with PCOS on liraglutide saw their periods return to normal. Over 40% started ovulating again - without fertility drugs. Testosterone levels dropped by 20-30%. Fasting insulin and HbA1c improved significantly. One woman on Reddit shared: “After six months on semaglutide, my testosterone fell from 68 to 42 ng/dL. I had my first regular period in three years.”
These aren’t isolated stories. Multiple trials confirm GLP-1s improve lipid profiles, reduce inflammation markers, and lower the risk of prediabetes turning into full-blown diabetes. In fact, one study showed a 70% remission rate of prediabetes in PCOS patients using GLP-1s - far higher than with metformin alone.
How Do They Compare to Other Treatments?
Metformin? It’s cheaper, safer long-term, and helps with insulin resistance. But it’s not great for weight loss. Oral contraceptives? They mask symptoms - they don’t fix the root problem. Bariatric surgery? It works, but it’s invasive and irreversible. GLP-1s sit in the middle: non-surgical, reversible, and powerful.
Here’s the breakdown:
| Treatment | Average Weight Loss | Metabolic Benefits | Cost (Monthly) | Side Effects |
|---|---|---|---|---|
| GLP-1 RAs (semaglutide) | 10-15% | High - lowers insulin, testosterone, inflammation | $800-$1,400 | Nausea, vomiting, dizziness (common) |
| GLP-1 RAs (liraglutide) | 5-10% | High - similar to semaglutide | $800-$1,200 | Nausea, injection site reactions |
| Metformin | 2-5% | Moderate - improves insulin sensitivity | $10-$20 | Diarrhea, bloating (usually mild) |
| Oral Contraceptives | 0-2% | Low - masks symptoms only | $0-$50 | Blood clots, mood changes, weight gain |
| Bariatric Surgery | 25-30% | Very high - long-term remission | $15,000-$25,000 (one-time) | Surgical risks, lifelong nutrient deficiencies |
GLP-1s win on effectiveness. But cost and side effects are real barriers.
Side Effects - What No One Tells You
Yes, they work. But they’re not easy to tolerate at first. About 44% of users get nausea. 24% vomit. 15% feel dizzy. Most side effects fade after 4-8 weeks as your body adjusts. Still, 15-20% of people quit because it’s too uncomfortable.
One woman on Reddit wrote: “Spent $1,200 a month on Wegovy. Lost 15 lbs. Couldn’t keep food down. Switched back to metformin.” That’s the trade-off. You’re paying a lot, feeling sick, and hoping the weight stays off.
There are also serious risks. GLP-1s are banned for people with a history of medullary thyroid cancer or multiple endocrine neoplasia. They’re not recommended during pregnancy. And while rare, there’s been concern about pancreatitis and gallbladder issues.
Who Benefits the Most?
GLP-1s work best for women with PCOS who have a BMI over 30 and signs of insulin resistance - high fasting glucose, high triglycerides, or acanthosis nigricans (dark patches on skin). They’re less effective in lean PCOS patients who don’t have metabolic issues.
If you’ve tried diet and exercise and still can’t lose weight, GLP-1s might be your next step. If you’ve been on metformin for years with little progress, they could be a game-changer. But if you’re under 30, don’t have insulin resistance, and just want to lose 10 pounds? You’re better off with lifestyle changes and maybe metformin.

How to Start - Practical Steps
Starting a GLP-1 isn’t like popping a pill. It’s an injection, usually once a week for semaglutide or daily for liraglutide. You inject it under the skin - belly, thigh, or arm. Most doctors start you low: 0.25 mg weekly for semaglutide. You increase slowly - every 4 weeks - until you hit the target dose (usually 1.7 mg or 2.4 mg).
Here’s what helps:
- Start with a low dose. Don’t rush to the top. Side effects drop sharply with slow titration.
- Drink plenty of water. Dehydration makes nausea worse.
- Eat small, low-fat meals. Greasy or sugary foods trigger nausea.
- Combine with metformin. Studies show women who stayed on metformin after stopping GLP-1s kept 2/3 of their weight loss. Those who stopped both regained 60-70%.
- Track your progress. Weigh weekly. Note changes in energy, periods, and cravings.
Insurance rarely covers GLP-1s for PCOS - they’re off-label. But some insurers will approve them if you have prediabetes or high BMI with complications. Always ask your doctor to submit a letter of medical necessity.
The Future - What’s Coming
In June 2024, the European Medicines Agency accepted Novo Nordisk’s application to approve semaglutide 2.4 mg specifically for PCOS. A decision is expected in early 2025. If approved, this could change everything - insurance coverage, prescribing norms, and access.
Oral GLP-1s like Rybelsus are already here. No needles. Just a daily pill. They’re less effective than injections, but easier to stick with. Combination drugs - like retatrutide, which targets three appetite hormones at once - are in trials and could double the weight loss.
Experts predict GLP-1s will become standard care for obese PCOS patients by 2027. But only if cost drops. Right now, they’re out of reach for most without good insurance.
Final Thoughts - Is It Worth It?
GLP-1s aren’t a cure for PCOS. They’re a tool. A powerful one. For women stuck in the cycle of weight gain, hormonal chaos, and failed diets, they offer real hope. The weight loss is real. The metabolic improvements are real. The return of periods? Real too.
But they’re expensive. They’re hard on the stomach. And you have to stay on them - stop, and most of the weight comes back. That’s why combining them with lifestyle changes is key. Don’t see them as a shortcut. See them as a bridge - to help you lose the weight so you can build habits that last.
If you’re considering GLP-1s, talk to an endocrinologist who understands PCOS. Ask about trials. Ask about financial assistance programs. Ask if metformin should be part of your plan. This isn’t a decision to make alone. But for many women, it’s the first time in years they’ve felt like their body might finally respond.
Do GLP-1s help with PCOS symptoms beyond weight loss?
Yes. Studies show GLP-1s improve menstrual regularity, reduce testosterone levels, increase ovulation rates, and lower insulin resistance. In one trial, 68% of women on liraglutide had regular periods after 24 weeks, and 42% ovulated spontaneously - without fertility treatments.
How long does it take to see results with GLP-1s for PCOS?
Most women notice reduced appetite and slight weight loss within 2-4 weeks. Noticeable weight loss (5% or more) usually happens by 12-16 weeks. Improvements in menstrual cycles and hormone levels often appear between 3 and 6 months.
Can I take GLP-1s if I’m trying to get pregnant?
GLP-1s are not recommended during pregnancy. If you’re planning to conceive, your doctor will likely advise stopping them at least 2 months before trying. However, losing weight with GLP-1s first can significantly improve your chances of natural conception and reduce pregnancy risks.
Are GLP-1s better than metformin for PCOS?
For weight loss and metabolic improvement, yes - especially if you have a BMI over 30. Metformin helps insulin resistance but only causes modest weight loss (2-5%). GLP-1s cause 5-15% weight loss and have stronger effects on hormones. However, metformin is much cheaper and safer for long-term use. Many doctors combine both.
Will I gain the weight back if I stop GLP-1s?
Most people do - unless they change their lifestyle. Studies show that stopping GLP-1s leads to weight regain of 60-70% within a year. But women who continue metformin and maintain diet/exercise habits after stopping GLP-1s regain only about one-third of the lost weight.
Is semaglutide approved for PCOS yet?
Not officially in the U.S. or Europe - yet. In June 2024, the European Medicines Agency accepted Novo Nordisk’s application for semaglutide 2.4 mg to treat obesity in women with PCOS. A decision is expected in early 2025. In the U.S., it’s still off-label, but many doctors prescribe it for PCOS based on strong evidence.