What Are Hormone Therapy Combinations?
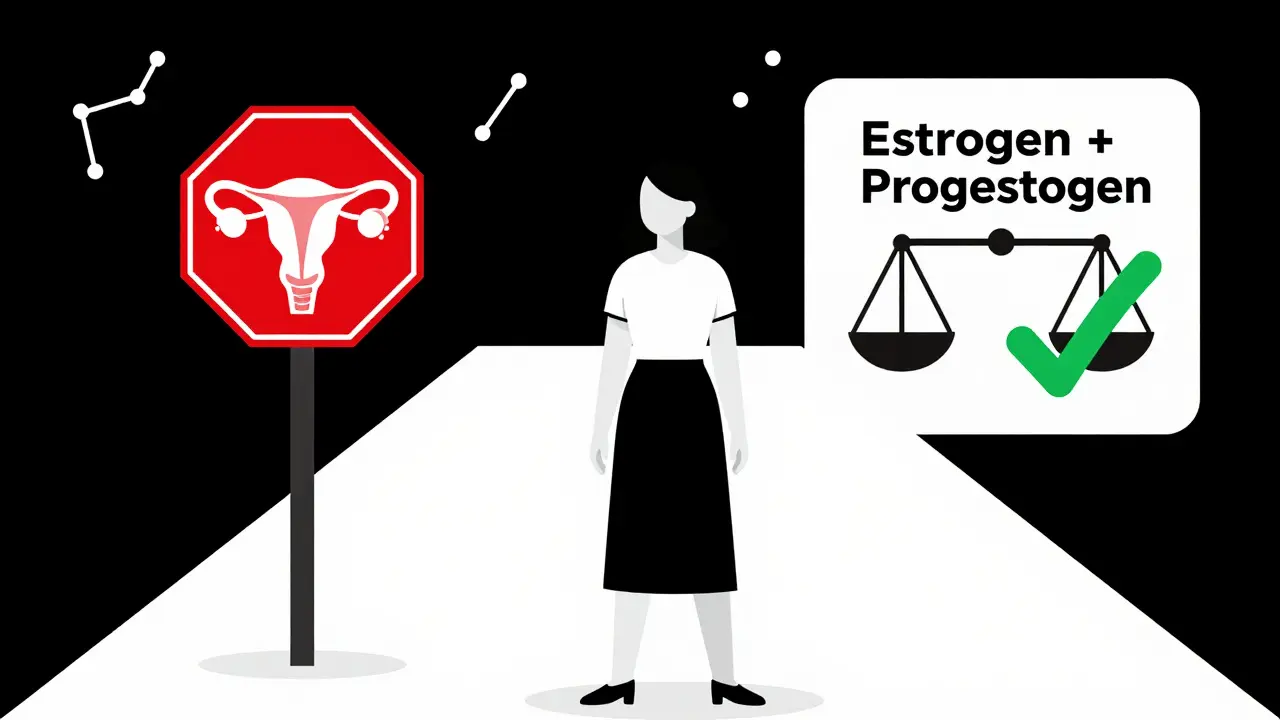
Hormone therapy combinations are used to replace hormones your body stops making during menopause. The most common mix is estrogen and progestogen. This isn’t just one-size-fits-all medicine-it’s tailored to your body’s needs, your health history, and whether you still have your uterus.
If you’ve had a hysterectomy, you only need estrogen. But if you still have a uterus, taking estrogen alone is dangerous. It can make the lining of your uterus grow too much, which can lead to cancer. That’s why doctors always pair estrogen with progestogen for women with a uterus. The goal? Relieve hot flashes, night sweats, and vaginal dryness-without putting you at higher risk for other problems.
Two Main Types: Sequential vs. Continuous
There are two main ways to combine these hormones, and which one you take depends on whether you’re still having periods or not.
Sequential combined HRT is for women who are still getting periods, or who’ve had their last period within the last year. You take estrogen every day, then add progestogen for the last 10 to 14 days of each month. This mimics your old cycle, and you’ll usually get a withdrawal bleed-like a period-each month. It’s designed for perimenopause, when your body is still adjusting.
Continuous combined HRT is for women who haven’t had a period for a full year. You take both estrogen and progestogen every single day, with no breaks. This stops periods completely and is the standard for postmenopausal women. It also lowers your risk of colon cancer by about 18% and type 2 diabetes by 21%, based on long-term data from the Women’s Health Initiative.
Generic Options: What’s Actually in Your Pills?
You don’t need to pay brand-name prices for effective treatment. Most hormone therapy prescriptions today are generic-and they work just as well.
- Conjugated estrogens (like Premarin generics): Available in 0.3mg, 0.45mg, and 0.625mg tablets. These are derived from horse urine and have been used for decades.
- Estradiol (the identical hormone your body makes): Comes in 0.5mg and 1mg tablets. Many doctors now prefer this because it’s bioidentical to human estrogen.
- Medroxyprogesterone acetate (a synthetic progestogen): Sold as 2.5mg, 5mg, and 10mg tablets. It’s cheap and widely available, but not the safest long-term option.
- Micronized progesterone (brand name: Prometrium, generics available): This is the natural form of progesterone. It’s more expensive than synthetic versions, but it’s gentler on your breasts and carries less cancer risk.
In the U.S., monthly costs for generics range from $4 to $40, depending on your insurance and pharmacy. In the UK, most are covered by the NHS and cost little to nothing out of pocket.
Delivery Methods Matter More Than You Think
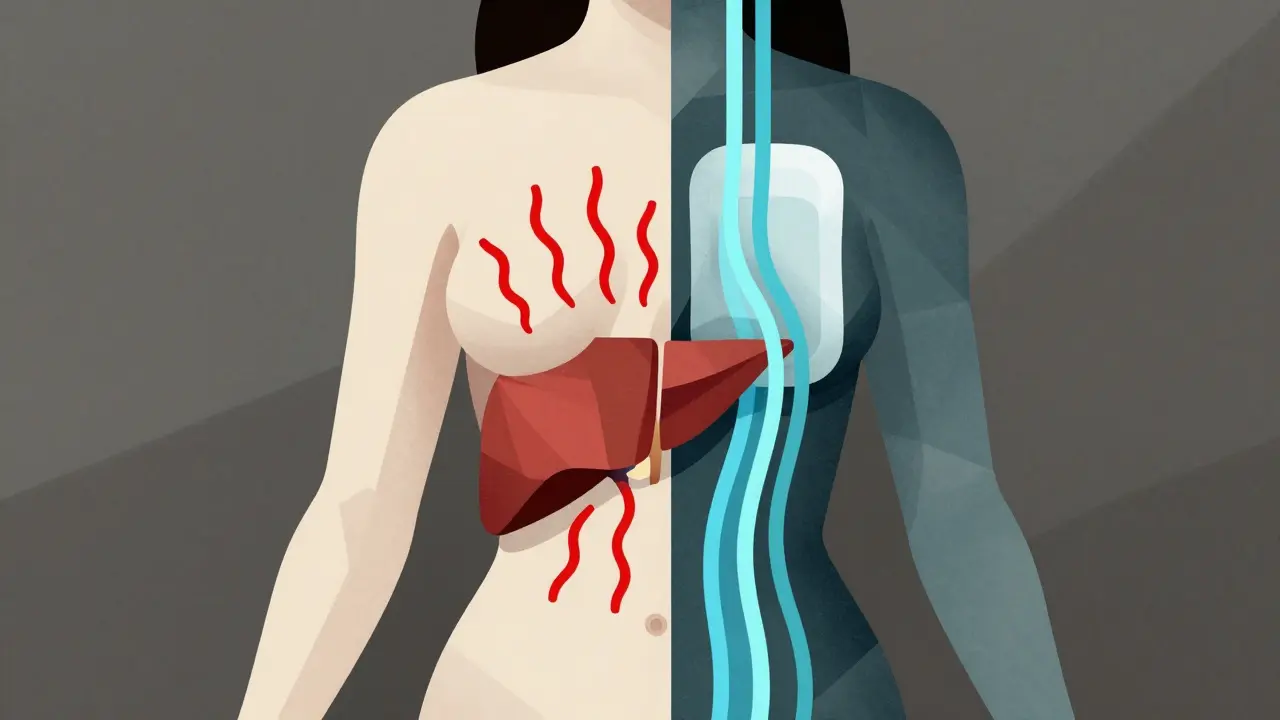
It’s not just about what hormones you take-it’s how you take them. The route of delivery changes your risk profile dramatically.
Oral tablets are the most common-but also the riskiest. When estrogen passes through your liver, it increases clotting factors. That raises your chance of blood clots, stroke, and pulmonary embolism. Studies show oral HRT increases venous thromboembolism (VTE) risk by 2 to 3 times compared to patches or gels.
Transdermal options (patches, gels, sprays) bypass the liver. They deliver estrogen directly into your bloodstream. That means:
- Lower risk of blood clots
- No increased stroke risk for women under 60
- Better safety for women with high blood pressure or a history of clotting
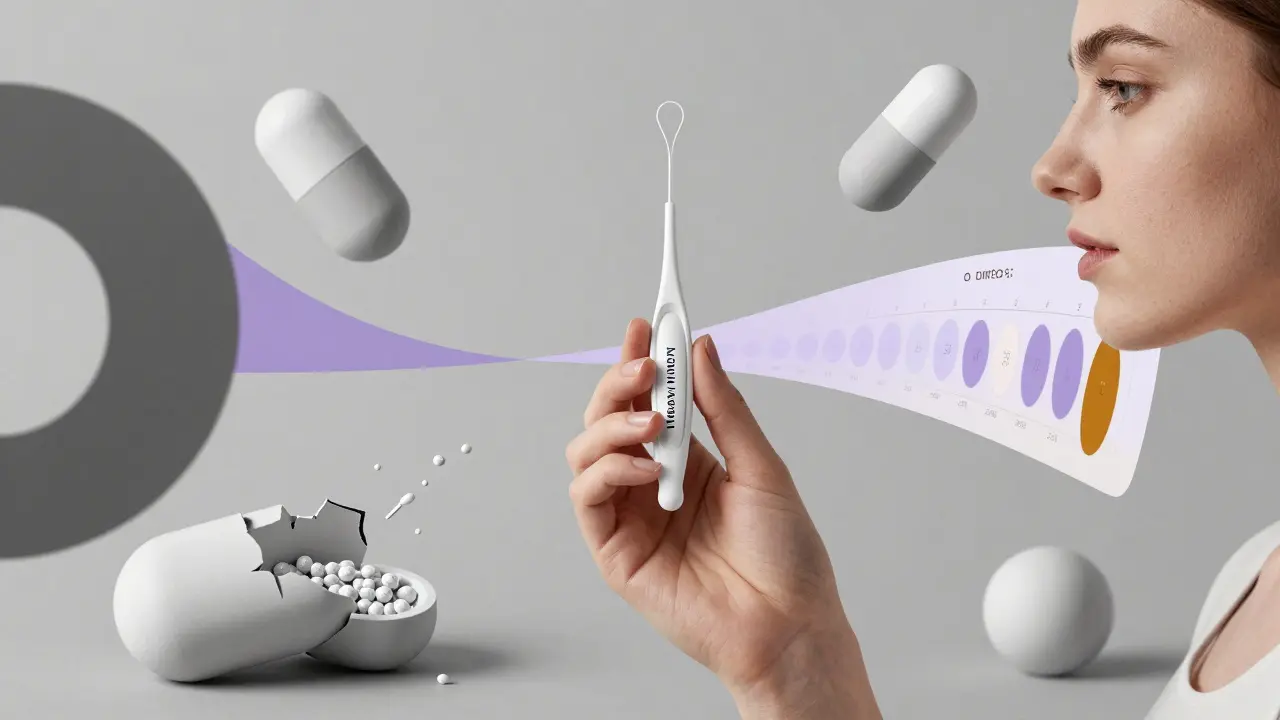
For progestogen, the best option is the Mirena IUS (intrauterine system). It releases progesterone directly into the uterus, so you don’t need to take a pill. This cuts systemic exposure and reduces breast cancer risk even further. Many women find this easier to manage long-term.
Who Should Avoid HRT? The Red Flags
HRT isn’t for everyone. There are clear situations where the risks outweigh the benefits.
- If you’ve had breast cancer, especially estrogen-receptor-positive-HRT is usually off-limits.
- If you’ve had a blood clot, stroke, or heart attack in the past year-avoid oral estrogen.
- If you have unexplained vaginal bleeding-you need a full workup before starting anything.
- If you’re over 60 and starting HRT for the first time-the risk of stroke and dementia goes up. Transdermal is safer, but still not recommended unless symptoms are severe and other options failed.
And here’s something many don’t realize: HRT is not for preventing heart disease, osteoporosis, or memory loss. The FDA and major medical groups (ACOG, NAMS, EMAS) all agree: it’s for symptom relief only.
Long-Term Use and Cancer Risk: The Real Numbers
Let’s talk about breast cancer. The fear is real-but the numbers are smaller than most think.
Using combined HRT for more than 5 years increases breast cancer risk slightly. For every 1,000 women using synthetic progestogens for 5 years, about 1 extra case of breast cancer occurs. That’s less than 1 in 1,000. With micronized progesterone, that number drops to about 0.7 extra cases per 1,000.
Compare that to the risk from being overweight, drinking alcohol, or not exercising. Those factors carry much higher cancer risks. The key is duration and type. If you use the lowest effective dose for the shortest time needed-usually 2 to 5 years-your risk stays very low.
Endometrial cancer is a bigger concern if you skip progestogen. In women with a uterus, estrogen-only therapy increases endometrial cancer risk by 2 to 12 times. That’s why it’s never prescribed unless you’ve had a hysterectomy.
Starting Out: What to Expect in the First 6 Months
Many women stop HRT because of side effects-but most of these are temporary.
Breakthrough bleeding is the most common reason. About 15-20% of women on continuous combined therapy will have spotting or light bleeding in the first 3 to 6 months. It’s usually harmless and goes away. But if it continues past 6 months, you need to see your doctor. It could mean your dose is too low, or you need to switch progestogen types.
Other common side effects:
- Breast tenderness (often from too much estrogen)
- Bloating or mood swings (can be linked to progestogen type)
- Headaches or nausea (especially with oral pills)
Start low. Go slow. Most doctors begin with the lowest dose of estradiol (0.5mg) and micronized progesterone (100mg daily) or a low-dose Mirena coil. Give it 3 months to settle. Adjust only if symptoms persist.
What’s New in 2026? The Future of HRT
The field is evolving fast. In 2023, the FDA approved a new transdermal patch that combines estradiol and micronized progesterone in one patch-called TWIRP. Early data suggests it may lower breast cancer risk compared to older oral combos.
Researchers are also testing new drugs like tissue-selective estrogen complexes (TSECs) and selective progesterone receptor modulators (SPRMs). These aim to give you the benefits of estrogen on bones and skin, without the cancer risk on breasts or uterus.
And the biggest shift? More women are choosing transdermal over oral. In Europe, 65% of prescriptions are now patches or gels. In the U.S., it’s still only 35%, but that’s climbing as doctors and patients learn the safety advantages.
Final Thoughts: It’s About Fit, Not Just Formula
Hormone therapy combinations aren’t about finding the ‘best’ product. They’re about finding the right one-for your body, your risks, and your life.
Ask yourself: Do I still have my uterus? Am I under 60 or within 10 years of menopause? Do I have a history of clots or breast cancer? Am I willing to use a patch or gel daily? Do I want to avoid monthly bleeding?
There’s no perfect answer. But there’s a good one for you. Work with your doctor. Test different options. Don’t be afraid to switch. And remember: you’re not taking hormones to live longer-you’re taking them to feel better while you live.
Can I use generic hormone therapy instead of brand-name?
Yes. Generic estrogen and progestogen tablets work just as well as brand names like Premarin or Provera. The FDA requires generics to have the same active ingredients, strength, and absorption rates. The only differences are in inactive fillers, which rarely affect how the medicine works. Most doctors prescribe generics because they’re cheaper and equally effective.
Is transdermal HRT safer than pills?
Yes, for most women. Patches, gels, and sprays deliver estrogen directly through the skin, avoiding the liver. This reduces the risk of blood clots, stroke, and gallbladder disease by up to 50% compared to oral pills. If you’re over 45, have high blood pressure, or are overweight, transdermal is usually the safer choice.
How long should I stay on hormone therapy?
There’s no fixed time limit. Most women use it for 2 to 5 years to manage menopause symptoms. After that, you should review your needs yearly. If hot flashes are gone, you might stop. If they return, you can restart at the lowest dose. The goal isn’t lifelong use-it’s symptom control during the transition.
What if I have a history of breast cancer?
HRT is generally not recommended if you’ve had estrogen-receptor-positive breast cancer. The hormones can stimulate cancer cells. Some women with severe symptoms may consider non-hormonal options like gabapentin or cognitive behavioral therapy. Always consult your oncologist before considering any hormone treatment.
Why does my doctor ask if I’ve had a hysterectomy?
Because estrogen alone can cause uterine lining to grow, which raises the risk of endometrial cancer. If you still have your uterus, you must take progestogen along with estrogen to protect your womb. If you’ve had a hysterectomy, you don’t need progestogen at all-just estrogen.