Many people take multiple medications every day - some for high blood pressure, others for thyroid issues, diabetes, or chronic pain. But what if taking two pills at the same time could make one of them useless - or even dangerous? It’s not rare. In fact, drug interactions are one of the leading causes of preventable hospital visits, and a big part of the problem isn’t the drugs themselves - it’s when you take them.
Why Timing Matters More Than You Think
Most people assume that if a doctor prescribes two medications, they’re safe to take together. But that’s not always true. Some drugs don’t interact because they’re incompatible - they interact because they’re taken at the same time. This is called a time-dependent drug interaction (TDDI). It’s not about the drugs clashing chemically in your body. It’s about timing. Take them too close together, and one can block the other from being absorbed, or change how your body processes it. For example, if you take an antacid like Tums or Maalox with ciprofloxacin (a common antibiotic), the calcium and magnesium in the antacid can bind to the antibiotic in your stomach. This stops the antibiotic from being absorbed. Studies show absorption can drop by up to 90%. But if you wait just two hours between them, the antibiotic works just fine. Same goes for levothyroxine (Synthroid), the thyroid medication millions rely on. If you take it with iron, calcium, or even coffee, absorption drops dramatically. Waiting four hours can preserve 95% of its effectiveness. The FDA says about 20-30% of all documented drug interactions can be avoided just by spacing out doses. That’s not a small number. That’s thousands of preventable side effects, hospitalizations, and treatment failures every year.Common Medications That Need Space
Not all drugs need timing adjustments. But some do - and missing the window can make your treatment fail. Here are the most common offenders:- Antibiotics (tetracycline, ciprofloxacin, levofloxacin): These bind to calcium, iron, magnesium, and aluminum. Don’t take them with dairy, antacids, or iron pills. Wait at least 2-3 hours before or after.
- Thyroid meds (levothyroxine): Absorbed only in the upper small intestine. Calcium, iron, soy, and even fiber supplements can block absorption. Take on an empty stomach, 30-60 minutes before food, and wait 4 hours before taking supplements.
- Bisphosphonates (alendronate, risedronate): Used for osteoporosis. Must be taken with a full glass of water, first thing in the morning, and you must stay upright for 30 minutes. No other meds or food for at least 30 minutes - or they won’t work.
- Statins (simvastatin, atorvastatin): Grapefruit juice can interfere with how your liver breaks them down. Even if you take them hours apart, grapefruit stays in your system. Avoid it entirely if you’re on these.
- Proton pump inhibitors (omeprazole, esomeprazole): Reduce stomach acid, which can affect absorption of other drugs like ketoconazole or iron. Separate by at least 2 hours if possible.
These aren’t just theoretical. A 2021 study in the Journal of Clinical Endocrinology & Metabolism found that patients who took levothyroxine with calcium supplements within 4 hours had thyroid hormone levels that were 25% lower than those who spaced them out. That’s enough to make symptoms like fatigue and weight gain come back - even if you’re taking the right dose.
What Timing Won’t Fix
Not every drug interaction can be solved by waiting. Some happen inside your liver, where enzymes break down drugs. If one drug blocks the enzyme that processes another, spacing them out won’t help. Take warfarin (a blood thinner) and metronidazole (an antibiotic). Metronidazole shuts down the liver enzyme (CYP2C9) that breaks down warfarin. This causes warfarin to build up in your blood, raising your risk of dangerous bleeding. No matter when you take them - even 12 hours apart - the enzyme is still blocked. The only solutions? Switch the antibiotic, lower the warfarin dose, or monitor your INR levels more closely. Same goes for statins and certain antifungals like ketoconazole, or antidepressants and antibiotics like clarithromycin. These are metabolic interactions. They’re not about absorption - they’re about chemistry inside your body. Timing doesn’t change that. You need a different drug, or a dose change.
How to Get It Right: A Simple 3-Step Plan
You don’t need to memorize every interaction. But you do need a system. Here’s how to start:- Make a full list of everything you take - prescriptions, over-the-counter pills, vitamins, supplements, even herbal teas. Include doses and times. Many people forget that magnesium supplements or calcium tablets can interfere.
- Check for known timing conflicts Use trusted resources like Lexicomp, Micromedex, or the FDA’s drug labeling database. If you’re unsure, ask your pharmacist. They have access to tools that flag these interactions instantly.
- Create a simple schedule Use a pill organizer with morning, afternoon, evening, and night compartments. Write down the required wait times next to each pill. For example: “Levothyroxine - take first thing, wait 4 hours before iron.”
One study found that using a color-coded pill box reduced timing errors by 43%. Another showed that patients who used the Medisafe app with custom alerts improved adherence to separation rules by 57%. Simple tools make a huge difference.
Why Doctors and Pharmacies Still Miss This
You’d think this would be automatic. But it’s not. Many electronic health records still don’t flag timing issues unless the drugs are taken at the exact same time. If you take your antibiotic at 8 a.m. and your antacid at 10 a.m., the system might not warn you - even though it’s too close. A 2023 survey by Medscape found that 78% of primary care doctors find managing multiple timed medications “moderately to severely difficult.” That’s because patients often see multiple specialists - one for heart disease, another for arthritis, another for depression. Each prescribes without knowing what the others have ordered. And most patients don’t tell their doctor about the vitamins they take. Worse, only 28% of outpatient clinics consistently write timing instructions on prescriptions. You might get a script for Synthroid, but no note saying “Take 4 hours before calcium.” You’re left guessing.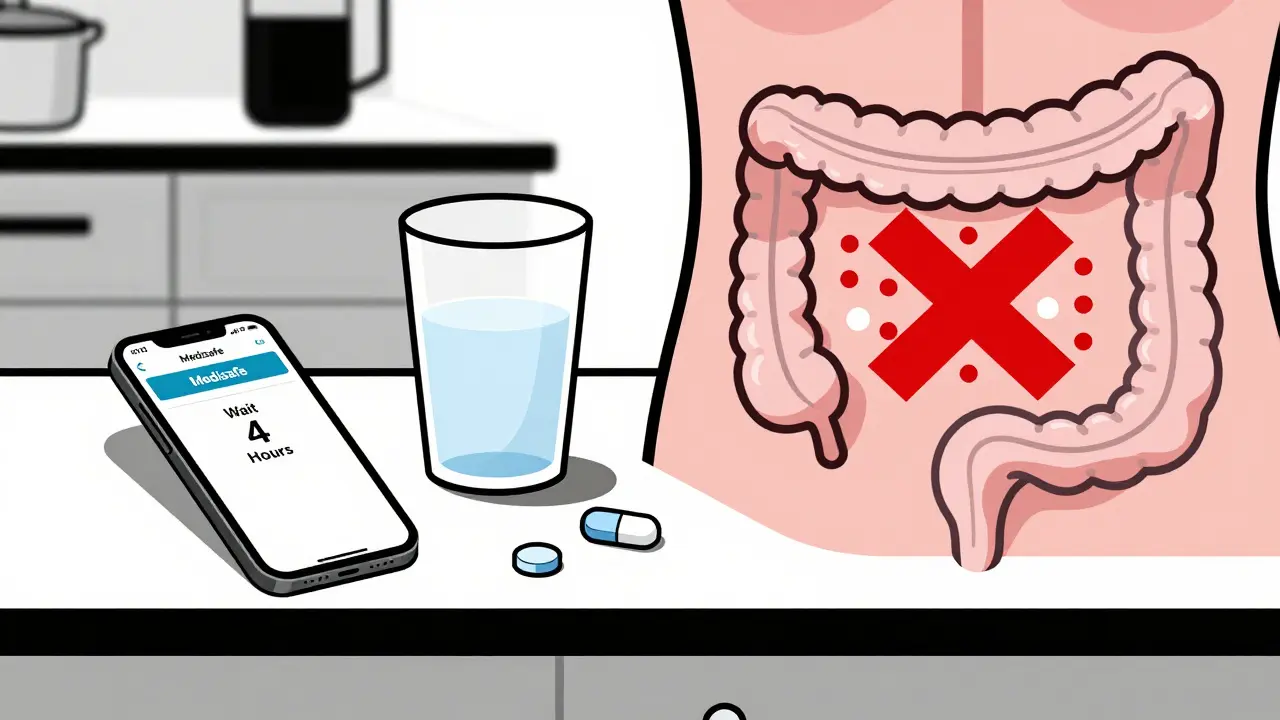
What Patients Are Really Struggling With
Real people face real problems. A 2022 survey of patients over 65 found that 68% said they “forget which meds need spacing” or “get confused when schedules conflict.” One woman took her thyroid pill with her morning coffee - and didn’t realize coffee blocks absorption. Her TSH levels stayed high for months. Another man took his iron pill with his blood pressure med - and ended up with severe anemia because the iron never got absorbed. The biggest hurdle isn’t knowledge - it’s complexity. If you’re on 8 or 10 medications, each with its own rule, it’s overwhelming. Nurses report spending 12-15 minutes per patient just to sort out timing schedules. And if you’re elderly, have memory issues, or live alone, it’s easy to mess up.What Works: Real Solutions That Help
There’s hope. The best strategies aren’t complicated:- Pill organizers with time slots: Use ones with 4-6 compartments. Label them clearly: “AM,” “Noon,” “PM,” “Bed.”
- Phone alerts: Apps like Medisafe, MyTherapy, or even Google Calendar can remind you when to take a pill - and when to wait. Set two alerts: “Take Synthroid” and “Wait 4 hours - now take iron.”
- Pharmacist check-ups: Ask your pharmacist to review your meds every 6 months. They can spot hidden timing conflicts you didn’t know about.
- One pharmacy: Fill all your prescriptions at the same place. That way, the pharmacist can see everything you’re taking and flag issues before you even leave.
At Kaiser Permanente, after implementing a full timing protocol across 40,000 providers, drug-interaction hospitalizations dropped by 29% in just one year. That’s not magic - it’s consistency.
What to Do Right Now
You don’t need to overhaul your life. Start small:- Look at your pill bottles. Do any say “take on empty stomach” or “avoid dairy”? If yes, note the timing rule.
- Write down your daily schedule. When do you take each pill? Is anything within 2 hours of something else?
- Call your pharmacist. Ask: “Are any of my meds timing-sensitive?”
- Download a free pill reminder app. Set alerts for both the pill and the wait time.
It’s not about being perfect. It’s about being aware. One small change - like waiting two hours between your antibiotic and antacid - can mean the difference between your treatment working… and failing silently.
Can I take my vitamins with my medications?
Some vitamins and supplements can interfere with medications - especially calcium, iron, magnesium, and zinc. These minerals can block absorption of antibiotics, thyroid meds, and bisphosphonates. Always check if your supplement contains these. If so, wait at least 2-4 hours between taking them and your medication. Multivitamins often contain these minerals, so read the label.
What if I forget to space out my meds?
If you take two interacting drugs too close together, don’t panic. Skip the next dose of one of them - but don’t double up later. For example, if you took your antibiotic and antacid together, skip the next antacid dose and wait until your next scheduled time. Never take extra doses to “make up” for a mistake. Contact your pharmacist or doctor if you’re unsure.
Do I need to avoid food with all my meds?
No - only specific ones. Thyroid meds, bisphosphonates, and some antibiotics work best on an empty stomach. But many drugs (like statins or blood pressure pills) are actually better taken with food to reduce stomach upset. Always check the label or ask your pharmacist. Don’t assume all meds should be taken without food.
Can my pharmacist help me organize my meds?
Yes - and they should. Pharmacists are trained to spot timing conflicts and can create a personalized schedule for you. Many offer free med reviews, especially if you take multiple prescriptions. Ask for a “medication therapy management” session. They’ll map out when to take each pill, what to avoid, and how to space them.
Are there apps that help with timing schedules?
Yes. Apps like Medisafe, MyTherapy, and Pill Reminder allow you to set multiple alerts per day - including “wait 2 hours” reminders. Some even sync with your pharmacy and send alerts if you miss a dose. A 2021 trial with 1,245 patients found these apps improved timing adherence by 57%. They’re free or low-cost and work on any smartphone.
Why do some drugs need 4 hours but others only 2?
It depends on how the drugs work in your body. Levothyroxine is absorbed quickly in the upper intestine, but calcium sticks around longer and can block absorption for hours. Antibiotics like ciprofloxacin bind to minerals fast, so 2 hours is enough to let them pass through. The exact timing comes from clinical studies that measure how long it takes for one drug to clear the absorption site before the next one can be effective.
If you’re taking more than three medications, timing isn’t just helpful - it’s essential. It’s not about being perfect. It’s about being smart. A few minutes of planning can save you from a hospital visit, a failed treatment, or worse. Talk to your pharmacist. Use a simple app. Write it down. Your body will thank you.
