When you’re living with rheumatoid arthritis, psoriasis, or severe eczema, the daily grind of pain, itching, and fatigue can wear you down. For many, biologic injections became the only real relief - until JAK inhibitors came along. These pills changed the game. No more needles. No more weekly clinic visits. Just a daily tablet that quietly shuts down inflammation from inside your cells. But here’s the catch: they come with serious risks you can’t ignore.
How JAK Inhibitors Actually Work
JAK inhibitors - also called jakinibs - don’t target single proteins like older biologics do. Instead, they block a whole signaling system inside immune cells called the JAK-STAT pathway. Think of it like cutting the wires in a control panel instead of unplugging one appliance. When cytokines (inflammatory signals) bind to receptors on your immune cells, JAK enzymes get activated. They turn on STAT proteins, which rush to the nucleus and tell your cells to make more inflammation. JAK inhibitors stop that before it starts.
There are four JAK enzymes: JAK1, JAK2, JAK3, and TYK2. Each one handles different cytokines. Drugs like upadacitinib and abrocitinib are picky - they mostly block JAK1, which is key for inflammation. Others like tofacitinib hit multiple JAKs, which makes them powerful but riskier. Ritlecitinib works differently: it binds permanently to JAK3 like a lock and key, shutting it down for good. That’s why it’s so effective for alopecia areata - hair loss from immune attacks on follicles.
The big win? Faster results. While biologics take 8 to 12 weeks to kick in, most people on JAK inhibitors feel better in 2 to 4 weeks. For someone with 18 swollen joints, that’s life-changing.
The Big Benefits: Convenience and Speed
Let’s be honest - the biggest reason people switch to JAK inhibitors is simple: they’re pills. No more freezing syringes. No more injecting yourself in the thigh before work. No more explaining to coworkers why you’re carrying a cold pack.
A 2023 survey of 1,247 patients found 92% preferred oral treatment over injections. Nearly 70% noticed symptom relief within two weeks. One Reddit user wrote: “Abrocitinib cleared my eczema in 10 days. I hadn’t slept through the night in years.” Another on HealthUnlocked said: “After failing three biologics, baricitinib cut my swollen joints from 18 to 2. I can hold my grandkids now.”
They also work across multiple conditions. Someone with rheumatoid arthritis and psoriasis can treat both with one pill. That’s huge. Before JAK inhibitors, you’d need separate drugs - or worse, multiple injections.
By 2023, JAK inhibitors made up about 25% of the rheumatoid arthritis treatment market. Global sales hit $12.3 billion. That’s not just hype - it’s real demand from real people tired of slow, painful treatments.
The Hidden Risks: Why Doctors Are Cautious
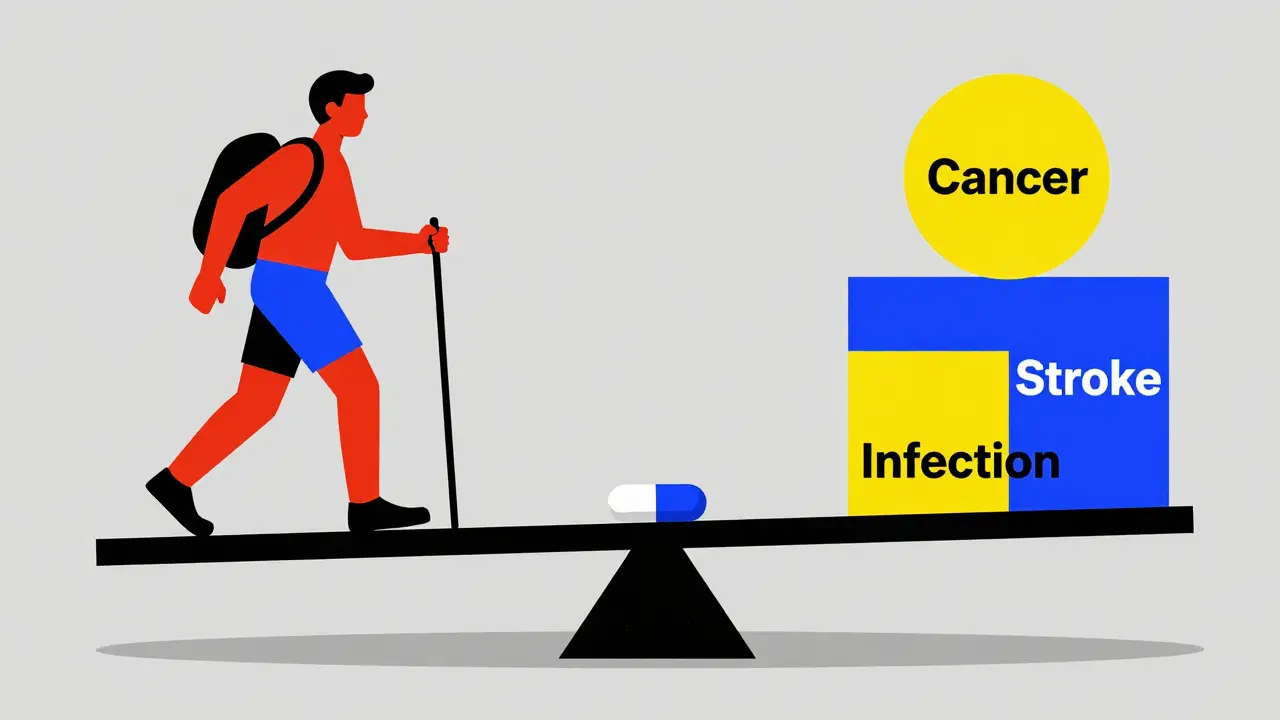
But here’s what no one tells you upfront: JAK inhibitors carry a black box warning from the FDA - the strongest possible alert. That means they can cause serious infections, cancer, heart attacks, strokes, and blood clots.
The ORAL Surveillance trial, a 5-year study of over 4,000 patients with rheumatoid arthritis, found those on tofacitinib had a 31% higher risk of major heart events and a 49% higher risk of cancer compared to those on TNF inhibitors. That risk doesn’t go away after a year - it keeps climbing. A 2024 follow-up showed the cancer risk stayed elevated even after 8.5 years.
Why? Because JAK enzymes aren’t just involved in inflammation. They help your body fight viruses, make red blood cells, and regulate cholesterol. Block them too broadly, and you’re messing with your body’s natural defenses.
Herpes zoster - shingles - is the most common serious side effect. About 23% of patients on JAK inhibitors get it, compared to just 3% on biologics. Many now take daily antivirals like valacyclovir just to prevent outbreaks. One patient said: “I got shingles twice in 10 months. Now I’m on medicine every day. I’m scared of what happens if I miss a dose.”
Lipid levels also rise. LDL (bad cholesterol) can jump by 28 mg/dL on average. That’s enough to push someone into high-risk territory for heart disease. Liver enzymes go up too. And blood counts? Lymphocytes can drop below 500 cells/μL - a red flag for serious infection risk.
Who Should - and Shouldn’t - Take Them
Not everyone is a candidate. The European League Against Rheumatism (EULAR) and American College of Rheumatology (ACR) both say: avoid JAK inhibitors if you’re over 65, have a history of heart disease, stroke, or cancer, or smoke. If you’ve had a blood clot, they’re off-limits.
They’re best for younger patients (under 65) with moderate-to-severe disease who’ve failed methotrexate and at least one biologic. If you’re healthy, active, and have no major risk factors, the benefits often outweigh the risks.
But here’s the problem: some doctors still prescribe them too early. In the U.S., 32% of rheumatologists use JAK inhibitors as first-line after methotrexate. In Europe, it’s only 18% - because they’re stricter about safety. The 2024 ACR/EULAR guidelines now say: JAK inhibitors should only be used when other options have failed and the patient has no cardiovascular or cancer history.
What You Must Monitor - And How Often
Taking a JAK inhibitor isn’t like taking a vitamin. You need regular blood tests. No exceptions.
Here’s what your doctor should check:
- Before starting: Complete blood count, liver enzymes (ALT/AST), lipid panel (cholesterol), tuberculosis test, and hepatitis B/C screening.
- Every 3 months for the first year: CBC, liver enzymes, lipids, and kidney function.
- Every 6 months after that: Same tests - don’t skip them.
Stop the drug if:
- Lymphocytes drop below 500 cells/μL
- Hemoglobin falls below 8 g/dL
- ALT or AST rises above 3 times the normal limit
- LDL cholesterol hits 190 mg/dL or higher (then start a statin)
And get vaccinated. The EMA recommends the shingles vaccine (Shingrix) at least 4 weeks before starting. But here’s the ugly truth: 68% of European clinics skip this because they’re in a rush to treat. Don’t be one of them.
The Future: Safer JAK Inhibitors on the Horizon
The next wave of JAK inhibitors is coming - and they’re designed to be smarter.
Deuruxolitinib, approved in June 2024 for alopecia areata, has a strict monitoring program built in. It’s the first to require enrollment in a REMS program - meaning you can’t get it without regular check-ins and blood work.
Even better: drugs like brepocitinib (a TYK2 inhibitor) are in phase 3 trials. They’re more selective. TYK2 is involved in inflammation but less so in blood cell production or cholesterol. Early data suggests fewer infections and no lipid spikes.
Ritlecitinib’s covalent binding to JAK3 might be the future - permanent inhibition means lower doses and fewer side effects. And deucravacitinib (already approved for psoriasis) works differently: it doesn’t block the active site. It changes the enzyme’s shape. That’s why it’s safer - and why it’s being tested for lupus and vitiligo.
By 2027, JAK inhibitors could capture 35% of the atopic dermatitis market. But only if the new, safer versions deliver on their promise.
Real Talk: Is It Worth It?
For some, yes. For others, no.
If you’re young, healthy, and your skin or joints are destroying your life - and you’ve tried everything else - JAK inhibitors can be a miracle. One patient told me: “I went from being bedridden to hiking with my daughter. I’ll take the risk.”
But if you’re over 60, have high blood pressure, smoke, or have a family history of cancer? Walk away. The risks aren’t theoretical. They’re documented. In the ORAL Surveillance trial, one in every 18 patients on tofacitinib had a major heart event or cancer diagnosis over five years.
And if your doctor doesn’t talk to you about monitoring? Get a second opinion. This isn’t a drug you take and forget. It’s a long-term commitment to blood tests, doctor visits, and self-awareness.
The bottom line: JAK inhibitors are powerful tools - not magic pills. They’re not for everyone. But for the right person, at the right time, they can give back a life.
Are JAK inhibitors better than biologics?
JAK inhibitors are better for convenience - they’re pills, not injections - and they work faster, often in 2 to 4 weeks. But biologics have a longer safety track record. JAK inhibitors carry higher risks of heart problems, cancer, and blood clots. For most patients without risk factors, JAK inhibitors are a strong option after one biologic fails. But if you’re at high risk for heart disease or cancer, biologics are still safer.
Can I stop taking JAK inhibitors if I feel better?
Don’t stop without talking to your doctor. Stopping suddenly can cause a flare-up of your condition - sometimes worse than before. Some patients can taper off under supervision, especially if they’ve been in remission for over a year. But many need to stay on long-term. Your doctor will decide based on your disease activity and test results.
Do JAK inhibitors cause weight gain?
Weight gain isn’t a direct side effect listed in trials. But many patients report gaining weight - often because their inflammation is under control and they can eat better, move more, or sleep better. Some also develop higher cholesterol or fluid retention, which can add pounds. If you notice sudden weight gain, check your blood pressure and kidney function - it could be a sign of fluid retention or high blood pressure.
Why do I need blood tests every 3 months?
JAK inhibitors affect your bone marrow, liver, and cholesterol production. Low white blood cells mean you’re more vulnerable to infections. High liver enzymes can signal damage. Rising cholesterol increases heart risk. These changes often happen without symptoms. Regular blood tests catch problems early - before they become dangerous.
Can I get the shingles vaccine while on a JAK inhibitor?
No. The shingles vaccine (Shingrix) is not live, so it’s safe to get before starting a JAK inhibitor. But once you’re on the drug, your immune system is suppressed. Getting the vaccine after starting can reduce its effectiveness and may not protect you. Always get vaccinated at least 4 weeks before beginning treatment. If you’ve already started, talk to your doctor about antiviral prevention instead.
What if I miss a dose?
If you miss one dose, take it as soon as you remember - unless it’s almost time for your next dose. Then skip the missed one. Don’t double up. Missing doses occasionally won’t cause immediate harm, but it can reduce effectiveness over time. If you miss more than two doses in a week, call your doctor. Your inflammation might be flaring, and you may need a temporary adjustment.
What Comes Next?
If you’re on a JAK inhibitor, stay on top of your labs. Don’t let busy life make you skip blood tests. Keep a log of your symptoms, energy levels, and any new rashes or infections. Talk to your doctor about vaccination status, cholesterol, and your personal risk factors.
If you’re considering one, ask: Am I healthy enough? Do I understand the risks? Is my doctor committed to monitoring me? If the answer isn’t a clear yes to all three, wait.
JAK inhibitors aren’t the end of the road - they’re a turning point. And like any powerful tool, they demand respect, not just reliance.
