Switching from a brand-name drug to a generic version is one of the most common changes in your medication routine - and for good reason. Generics cost less, often by 80% or more, and they’re just as safe and effective for most people. But that doesn’t mean you can just swap them and forget about it. Monitoring your health after switching to generics isn’t about doubting the science - it’s about paying attention to your body. Because while the FDA says generics are bioequivalent, your body might react differently. And that’s okay. It’s not a failure. It’s data.
Why You Might Notice a Difference
The FDA requires generic drugs to deliver the same amount of active ingredient into your bloodstream as the brand-name version, within the same timeframe. That’s called bioequivalence. To prove it, manufacturers must show that the concentration of the drug in your blood (measured as AUC and Cmax) falls between 80% and 125% of the brand-name drug. Sounds tight, right? It is. But that still leaves room for small variations in how your body absorbs the medicine. These differences aren’t about quality. Generic pills use the same active ingredient. But they can have different fillers, dyes, or coatings - things that don’t treat your condition but can affect how quickly the pill breaks down in your stomach. For most people, that’s invisible. For others, especially those on drugs with a narrow therapeutic index, it can matter. Drugs like warfarin (for blood thinning), levothyroxine (for thyroid), and lamotrigine (for seizures) have very little room for error. Too little, and the drug doesn’t work. Too much, and you risk serious side effects. That’s why doctors and health organizations like the American Heart Association and the American Academy of Family Physicians recommend extra monitoring after switching.What to Watch For
You don’t need to become a lab technician. But you do need to track a few key things - especially in the first 30 to 90 days after switching.- Symptoms returning or worsening: If you’re on medication for high blood pressure, diabetes, epilepsy, or depression, pay attention. Are your headaches coming back? Are your mood swings worse? Did your blood sugar spike unexpectedly? These aren’t just "bad days." They’re signals.
- New side effects: Did you start feeling dizzy, nauseous, or unusually tired after the switch? It could be the new filler in the pill. It could also be your body adjusting. Either way, write it down.
- Changes in how the pill looks or feels: Generics come from different manufacturers. One month it’s a white oval, the next it’s a blue capsule. That’s normal. But if the new pill tastes bitter, doesn’t dissolve the same way, or gives you stomach upset where the old one didn’t - note it.
How to Track Your Health
Start simple. Keep a notebook or use a free app on your phone. Log:- When you take your medicine
- Any symptoms you notice (good or bad)
- Relevant measurements - blood pressure, blood sugar, seizure count, peak flow for asthma
- Thyroid (levothyroxine): Get a TSH blood test at 6 weeks after switching. The American Thyroid Association says this is the best window to catch changes.
- Diabetes: Check your HbA1c at 4 and 8 weeks. If it’s up more than 0.5%, talk to your doctor.
- High blood pressure: Take readings twice a week for the first month. If your average systolic pressure jumps by 10 points or more, it’s time to call.
- Epilepsy or bipolar disorder: Track seizure frequency or mood episodes daily for 30 days. If you have more than one breakthrough event, don’t wait.
Which Generics Need Extra Caution
Not all generics are created equal when it comes to risk. The FDA and independent researchers have flagged a few categories where switching has led to more reports of issues:- Levothyroxine: 12% of people switching thyroid meds report changes in energy, weight, or heart rate. Even small shifts in absorption can throw off hormone balance.
- Lamotrigine: Used for seizures and bipolar disorder. 9% of switchers in Consumer Reports’ 2023 survey reported increased seizures or mood instability.
- Bupropion: An antidepressant and smoking cessation aid. Some users report altered mood or sleep patterns after switching brands.
- Warfarin: Even tiny changes in blood levels can lead to dangerous bleeding or clots. The American Heart Association recommends INR checks at 7 and 30 days after switching.
What to Do If Something Feels Off
If you notice a real change - not just a feeling, but a measurable one - don’t assume it’s "all in your head."- Don’t stop taking the medicine. That’s dangerous.
- Don’t switch back on your own. You might end up with a different generic version.
- Do call your doctor. Bring your symptom log. Mention the generic manufacturer’s name - it’s on the pill bottle.
How to Verify Your Generic
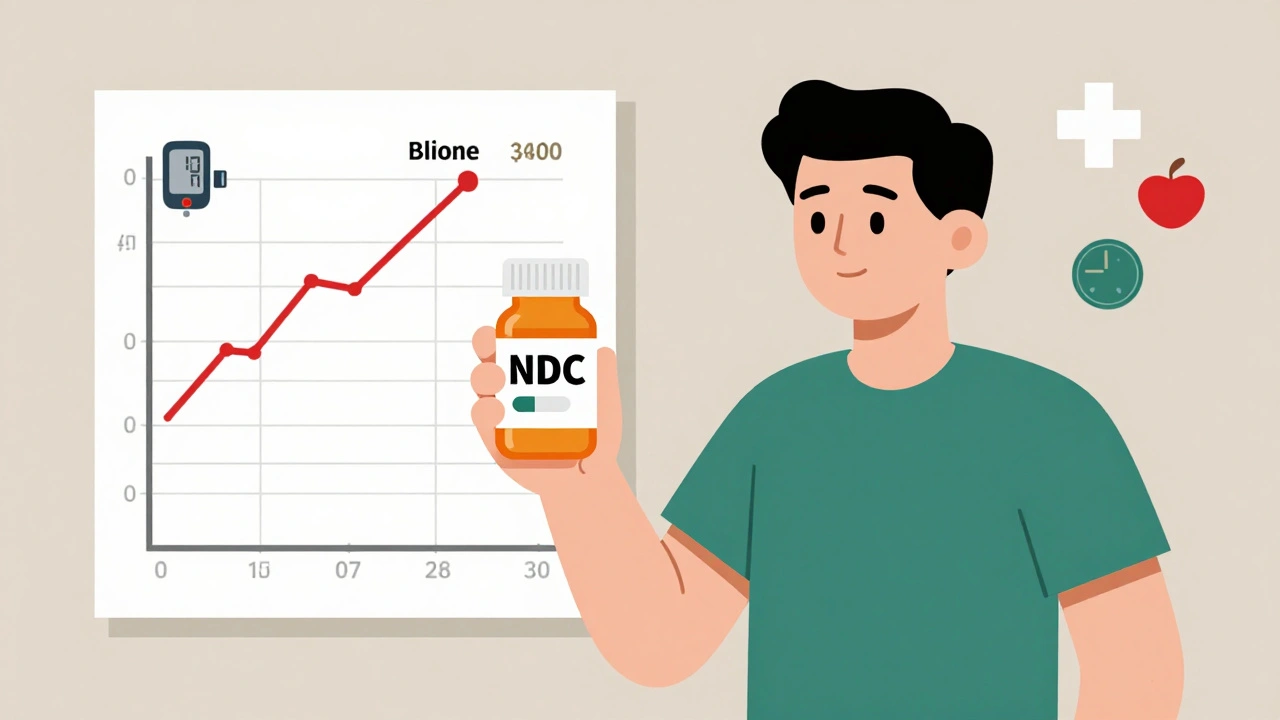
Every pill has a National Drug Code (NDC) - a unique 10-digit number on the packaging. It tells you exactly which company made it and what batch it came from. If you get your refill and the NDC changes, that’s a new manufacturer. That’s normal. But if you notice symptoms after the NDC changed, that’s your clue. Write down the NDC and keep a copy of the bottle. If you report an issue later, this number is critical. You can also check the FDA’s Orange Book online (or ask your pharmacist) to see if your drug has a therapeutic equivalence rating of "AB." That means it’s approved as interchangeable. Some drugs have "BX" ratings - meaning they’re not automatically interchangeable. That’s rare, but it happens.
When to Report a Problem
The FDA’s MedWatch program collects reports from patients like you. In 2022, they got over 1.2 million reports - and only 15% were about generics. But among those, 62% involved epilepsy drugs, and 28% involved heart meds. If you have a serious issue - hospitalization, new seizure, dangerous drop in blood pressure - report it. You don’t need to prove anything. Just describe what happened, when, and what drug you took. Go to www.fda.gov/medwatch or call 1-800-FDA-1088. The FDA commits to reviewing serious reports within 30 days. Your report could help someone else.Most People Don’t Notice a Thing
Let’s be clear: the vast majority of people who switch to generics feel no difference at all. Data from PatientsLikeMe shows 92.7% of 42,000+ switchers maintained the same level of symptom control. Consumer Reports found 89% were satisfied. You’re not alone if you notice something. But you’re also not broken. Your body is just different. And that’s why monitoring matters.Final Advice: Stay Informed, Not Afraid
Generics saved the U.S. healthcare system $373 billion in 2022. They’re not a compromise - they’re a smart choice. But smart choices require awareness. Take your medicine as prescribed. Track your symptoms. Know your NDC. Talk to your doctor. Report anything unusual. You’re not being paranoid. You’re being responsible. The science says generics work. Your body tells you if they’re working for you. Listen to both.Are generic medications really as effective as brand-name drugs?
Yes, for most people and most medications, generics are just as effective. The FDA requires them to deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. Over 90% of prescriptions in the U.S. are generics, and studies show they work just as well for conditions like high blood pressure, cholesterol, and infections. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or certain seizure meds - small differences in absorption can matter. That’s why monitoring is important for those specific cases.
How long should I monitor my health after switching to a generic?
For most people, 30 days is enough to see if there’s a change. But for medications with narrow therapeutic indices - such as thyroid, blood thinners, or epilepsy drugs - experts recommend monitoring for 60 to 90 days. Blood tests (like TSH for thyroid or INR for warfarin) should be done at 4 to 6 weeks. If symptoms return or worsen within that time, contact your doctor. Don’t wait until your next scheduled visit.
Can I switch back to the brand-name drug if I don’t feel right?
Yes, but don’t do it without talking to your doctor first. Sometimes, switching to a different generic manufacturer solves the issue - not going back to the brand. Your doctor can write a prescription that says "Dispense as Written" or "Do Not Substitute," which prevents the pharmacy from switching you again. Insurance may require prior authorization for the brand-name drug, but many will approve it if there’s documented medical need.
Why do some generics look different from others?
Generic manufacturers can’t copy the exact look of brand-name pills because of trademark laws. So they change the color, shape, or size. That’s normal. But if you notice a change in how the pill tastes, how quickly it dissolves, or if you start having new side effects after the appearance changed - that’s worth noting. It could mean you’ve switched to a different manufacturer with a different filler or coating. Write down the NDC number on the bottle to track which version you’re taking.
What should I do if I think my generic isn’t working?
First, don’t stop taking it. Second, track your symptoms and any changes in your condition. Keep a log of dosing times, symptoms, and measurements like blood pressure or blood sugar. Then, call your doctor. Bring your log and the pill bottle with the NDC number. Your doctor may order a lab test to check drug levels or switch you to a different generic brand. If you’ve had a serious reaction, report it to the FDA through MedWatch - your report helps improve safety for everyone.