When you’ve got a throbbing headache, a sore back, or stiff knees, you probably reach for the medicine cabinet. But do you grab ibuprofen or Tylenol? It’s not just brand preference-it’s about what’s actually happening in your body. NSAIDs and acetaminophen are the two most common over-the-counter pain relievers, but they work in completely different ways. Choosing the wrong one won’t just mean slower relief-it could put your health at risk.
How They Work: Two Different Paths
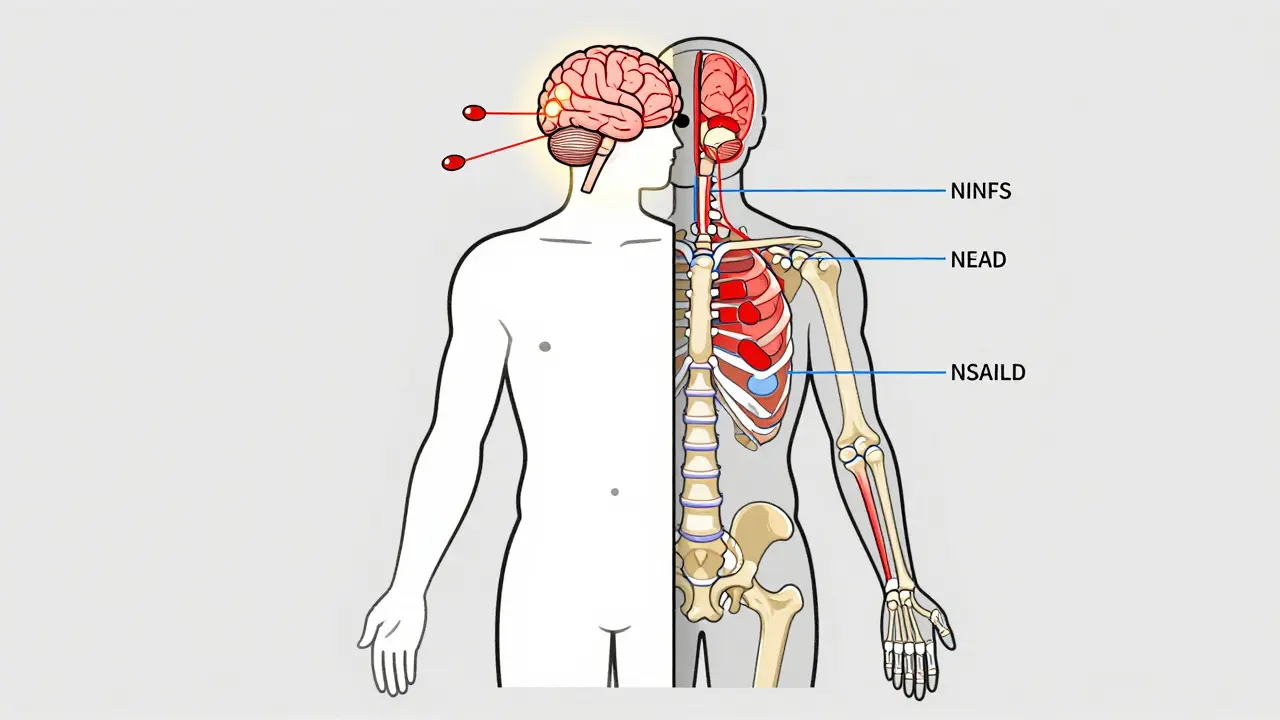
Acetaminophen, the active ingredient in Tylenol, doesn’t touch inflammation. That’s why it’s good for headaches, fever, or aching muscles without swelling. It works mostly in your brain and spinal cord, blocking pain signals. Scientists still aren’t 100% sure how, but it’s clear: if there’s no swelling, acetaminophen does a solid job.
NSAIDs-like ibuprofen (Advil, Motrin) and naproxen (Aleve)-are different. They stop your body from making prostaglandins, chemicals that cause pain, fever, and inflammation. That’s why they’re the go-to for sprained ankles, arthritis, or menstrual cramps. When tissue is swollen, red, or hot to the touch, NSAIDs get to the root of the problem.
This difference isn’t just academic. If you have a pulled muscle with swelling, acetaminophen might help the pain, but it won’t calm the inflammation. NSAIDs will. But if you have a stomach ulcer or high blood pressure, NSAIDs could make things worse.
What’s Safe? The Real Risks
Both medications are safe when used as directed-but push the limits, and trouble follows.
Acetaminophen’s biggest danger is your liver. The maximum daily dose is 4,000 milligrams. That sounds like a lot-until you realize many cold and flu medicines also contain it. Taking Tylenol for a headache, then a cold tablet an hour later? You could easily hit 5,000 mg without meaning to. The FDA says this causes about 56,000 emergency room visits and 425 deaths every year in the U.S. alone. That’s why experts now recommend capping intake at 3,000 mg daily, especially if you drink alcohol or have liver issues.
NSAIDs have their own red flags. They irritate the stomach lining, leading to ulcers and bleeding in 10-20% of regular users. Long-term use raises the risk of heart attack and stroke, especially in people over 60 or with existing heart disease. Naproxen carries slightly less cardiovascular risk than ibuprofen, but neither is risk-free. And if you’re on blood thinners like warfarin, NSAIDs can make bleeding more likely.
Here’s a quick comparison:
| Feature | NSAIDs (Ibuprofen, Naproxen) | Acetaminophen (Tylenol) |
|---|---|---|
| Reduces inflammation? | Yes | No |
| Best for | Swelling, arthritis, sprains, menstrual pain | Headaches, fever, general aches |
| Max daily OTC dose | 1,200 mg (ibuprofen), 660 mg (naproxen) | 4,000 mg (but 3,000 mg recommended) |
| Main risk | Stomach bleeding, heart strain, kidney stress | Liver damage from overdose |
| Safer with blood thinners? | No | Yes |
When to Choose Which One
It’s not about which is "better." It’s about which fits your situation.
If you have osteoarthritis in your knee, NSAIDs are more effective. A 2023 review from the Hospital for Special Surgery found acetaminophen barely outperformed placebo for joint pain. But if you’ve got a tension headache, NSAIDs might give you stomach upset, while acetaminophen gets you back on track with no side effects.
For back pain? If it’s from lifting something heavy and you feel swelling, go with ibuprofen. If it’s just stiffness with no redness or heat, acetaminophen is fine.
For menstrual cramps? NSAIDs are usually the winner-they reduce the prostaglandins that cause uterine contractions. Acetaminophen helps, but less reliably.
And if you’re unsure? Start with acetaminophen. It’s gentler on your stomach and safer if you have heart or kidney issues. But if it doesn’t help after a day or two, switching to an NSAID might be the answer.
Combining Them? It’s Actually Smart
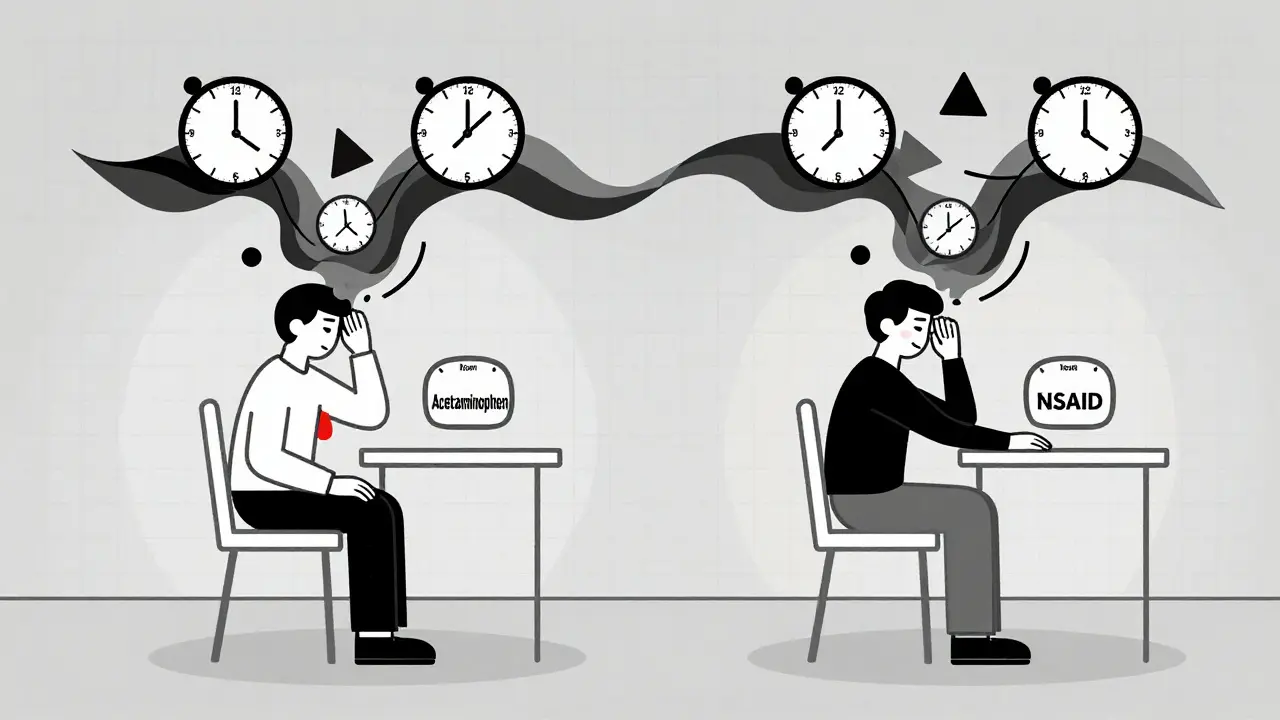
Many people think you should pick one or the other. But doctors increasingly recommend using both-strategically.
Studies show that taking acetaminophen and an NSAID together gives better pain relief than either alone, with lower total doses. That means less risk for both liver and stomach damage.
Here’s how a common schedule looks:
- 8 a.m.: 500 mg acetaminophen
- 2 p.m.: 200 mg ibuprofen
- 8 p.m.: 500 mg acetaminophen
- 10 p.m.: 200 mg ibuprofen
This keeps pain under control without overloading either system. It’s especially useful for chronic pain like lower back pain or osteoarthritis.
Just remember: don’t mix NSAIDs with aspirin if you’re taking it for heart protection. Ibuprofen can block aspirin’s blood-thinning effect. Talk to your doctor if you’re on daily low-dose aspirin.
What You Should Never Do
- Don’t take more than the recommended dose, even if the pain is bad. More isn’t better-it’s dangerous.
- Don’t combine multiple pain relievers without checking labels. Cold medicines often contain acetaminophen. Taking Tylenol on top of that? You’re asking for liver trouble.
- Don’t use NSAIDs for more than 10 days straight without seeing a doctor. Same goes for acetaminophen beyond 10 days.
- Don’t drink alcohol while taking either. It increases liver damage risk with acetaminophen and stomach bleeding risk with NSAIDs.
- Don’t assume "natural" or "herbal" pain relievers are safer. Many interact with these medications in unpredictable ways.
Bottom Line: Know Your Body, Know Your Medicine
There’s no one-size-fits-all pain reliever. Acetaminophen is your friend for headaches, fever, or general aches-especially if you have stomach, heart, or kidney issues. NSAIDs are your best bet for anything with swelling: arthritis, sprains, tendonitis, or menstrual cramps.
The smartest move? Use the lowest dose that works. Don’t take either daily unless you’ve talked to your doctor. And if you’re combining them, stick to a schedule. Many people find alternating every 4-6 hours gives them steady relief without the risks.
And if you’re not sure? Ask. A pharmacist can help you read labels. Your doctor can help you weigh risks based on your health history. Pain relief shouldn’t come with hidden costs.
Can I take acetaminophen and ibuprofen together?
Yes, under the right conditions. Taking them together can provide better pain relief than either alone, especially for moderate to severe pain. The key is spacing them out-take one, wait 4-6 hours, then take the other. Never exceed the daily maximum for either: 3,000-4,000 mg for acetaminophen and 1,200 mg for ibuprofen. Always check other medications you’re taking, as many cold and flu products contain acetaminophen.
Which is safer for long-term use?
For most people, acetaminophen is safer for long-term use-if you stay under 3,000 mg per day and avoid alcohol. NSAIDs carry higher risks over time: stomach ulcers, kidney damage, and increased heart attack or stroke risk. But if your pain comes from inflammation (like arthritis), NSAIDs may be necessary. Always discuss long-term use with your doctor, especially if you have liver, kidney, or heart conditions.
Why does acetaminophen not work for my arthritis pain?
Arthritis pain often involves inflammation in the joints. Acetaminophen reduces pain signals in the brain but doesn’t touch inflammation. NSAIDs, on the other hand, block the chemicals that cause swelling, redness, and heat. That’s why studies show NSAIDs like ibuprofen or naproxen are significantly more effective for osteoarthritis than acetaminophen. If acetaminophen isn’t helping, switching to an NSAID may be the solution.
Is Tylenol better than ibuprofen for headaches?
For most tension headaches or migraines, yes. Tylenol is often preferred because it doesn’t irritate the stomach like ibuprofen can. It also doesn’t interfere with blood pressure medications or blood thinners. However, if your headache is linked to inflammation (like sinus pressure or a recent injury), ibuprofen might work better. Try both and see which gives you relief without side effects.
Can I use NSAIDs if I have high blood pressure?
Use caution. NSAIDs can raise blood pressure and reduce the effectiveness of some blood pressure medications. If you have hypertension, acetaminophen is usually the safer first choice. If you need an NSAID, naproxen may carry less cardiovascular risk than ibuprofen-but still consult your doctor before using it regularly. Never take NSAIDs daily without medical advice if you have heart disease or high blood pressure.