When someone is struggling with obsessive-compulsive disorder (OCD), finding the right medication can feel like searching for a key in a dark room. You know it’s out there, but every turn feels risky. The truth? Two types of medication have stood the test of time: SSRIs and clomipramine. They’re not magic pills, but they’re the only ones with solid, science-backed proof of helping people reduce obsessive thoughts and compulsive behaviors. And how you take them? That matters just as much as which one you choose.
Why SSRIs Are the First Choice
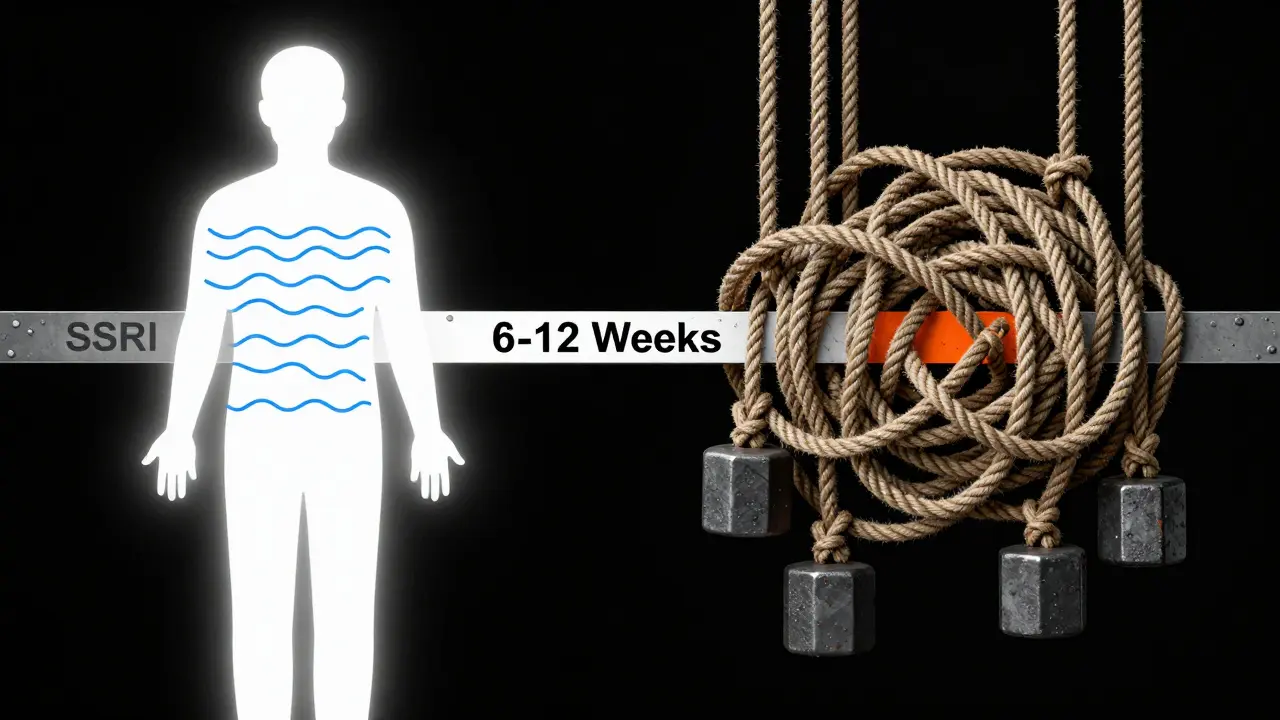
Selective serotonin reuptake inhibitors - or SSRIs - are the go-to starting point for most doctors treating OCD. Why? Because they work, and they’re generally easier to live with. Medications like sertraline, fluoxetine, fluvoxamine, and paroxetine were originally developed for depression, but research showed they’re even more effective for OCD when given at higher doses.Here’s the catch: the dose for OCD is not the same as for depression. If you’re on 20 mg of sertraline for sadness, that won’t touch your OCD. For OCD, most people need 200-300 mg daily. That’s three to four times higher than what’s used for depression. Fluoxetine? Same story. For depression, 20 mg is typical. For OCD, you’re looking at 40-60 mg. Paroxetine? 40-60 mg for OCD, not the 10-20 mg used for anxiety.
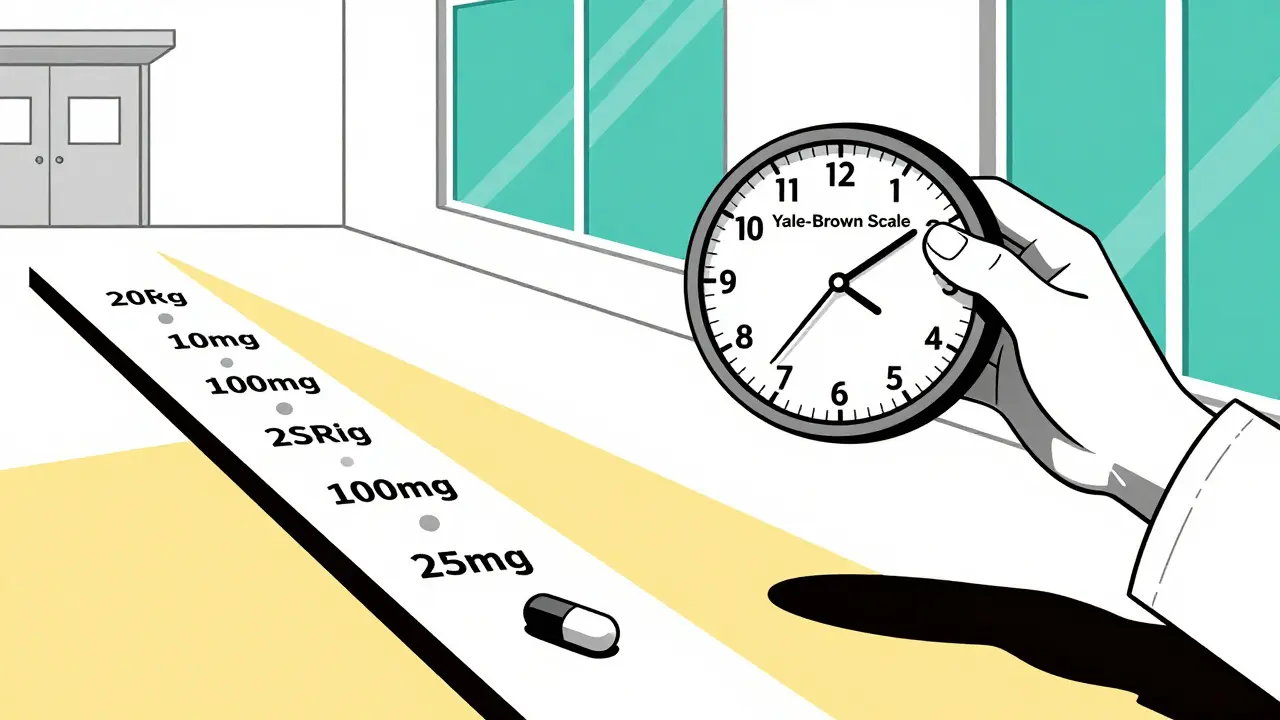
It takes time. You won’t feel better in a week. Most studies show you need at least eight to twelve weeks on a full dose before you can tell if it’s working. And even then, improvement is gradual. A 25-35% drop in symptoms - measured by the Yale-Brown Obsessive Compulsive Scale - is considered a good response. That means if your compulsions used to take up five hours a day, you might drop to three. Not zero. But enough to breathe again.
Side effects? Yes. Nausea, insomnia, sexual dysfunction, jitteriness. But these usually fade after the first few weeks. The big advantage? SSRIs don’t mess with your heart like older drugs do. No need for regular ECGs unless you’re on a very high dose. And if one SSRI doesn’t work? Try another. About 60% of people who don’t respond to one SSRI will respond to another.
Clomipramine: The OG OCD Drug
Clomipramine - sold under the brand name Anafranil - was the first medication ever approved by the FDA specifically for OCD, back in 1989. It’s a tricyclic antidepressant, older and more powerful than SSRIs. And yes, it still works. In fact, some studies show it’s slightly more effective than SSRIs, especially in kids and teens. One meta-analysis found clomipramine improved OCD symptoms by 37% in children, outperforming sertraline and fluoxetine.But here’s the trade-off: side effects. Clomipramine hits your body harder. Dry mouth? Constant. You’ll need to sip water all day. Weight gain? Common - 15-25 pounds in six months isn’t unusual. Drowsiness? So bad some people can’t drive. And then there’s the heart. Clomipramine can lengthen the QTc interval on an ECG, which raises the risk of dangerous heart rhythms. That’s why doctors monitor it closely - especially if you’re over 150 mg a day.
Dosing is precise. For adults, you start at 25 mg a day, usually at night because it makes you sleepy. Then you increase by 25 mg every 4-7 days. Most people need 100-250 mg daily. The max? 250 mg. For kids 10 and older, it’s 1-3 mg per kg of body weight, max 200-250 mg. Elderly patients? Start at 10 mg. Go slow. Their bodies process it differently.
Some patients swear by it. Reddit users report that after failing four or five SSRIs, clomipramine at 175 mg finally stopped their checking rituals. But 43% of those who tried it quit because the side effects were too much. It’s not for everyone. But for the person who’s tried everything else? It’s often the last resort that works.
Dosing: It’s Not One-Size-Fits-All
You can’t just pick a number and hope for the best. Dosing is a slow dance. Rushing it makes things worse.For SSRIs, doctors usually start low: 12.5 mg of sertraline, or 25 mg of fluvoxamine. Then they bump it up by 25-50 mg every week. Why so slow? Because the first two weeks can make OCD symptoms feel worse. Anxiety spikes. Compulsions intensify. It’s terrifying. But 89% of people who stick it out see improvement by week four. That’s why doctors tell you: don’t quit. You’re not broken. You’re adjusting.
Clomipramine? Even slower. Start at 25 mg. Wait four days. Then go to 50 mg. Then 75 mg. You might not hit 100 mg until week six. Some people take 10-14 weeks to reach their target. Blood tests aren’t routine, but if you’re over 75 mg, your doctor might check your plasma levels. Responders usually hit 220-350 ng/mL of clomipramine and 379 ng/mL of its metabolite, desmethylclomipramine. That’s the sweet spot.
Timing matters too. Both SSRIs and clomipramine are often taken at night. Clomipramine? Always at night - the drowsiness is too strong to risk daytime. SSRIs? Sometimes. If they make you sleepy, take them at night. If they make you jittery? Morning. Your doctor will help you find the rhythm.
Who Gets What? Clinical Guidelines in Practice
The American Psychiatric Association’s 2020 guidelines are clear: try two full SSRI trials before even thinking about clomipramine. That means 12 weeks on each, with at least six weeks at the highest dose you can tolerate. If neither works? Then clomipramine enters the picture.But here’s what happens in real life. In the U.S., 85% of first prescriptions for OCD are SSRIs. Sertraline leads at 32%, followed by fluvoxamine at 28%. Clomipramine? Only 8% of initial prescriptions. But that jumps to 22% when someone’s tried two SSRIs and still struggles. It’s not a first-line drug - it’s a second-line lifeline.
There’s also a growing trend: combining SSRIs with low-dose clomipramine. Instead of switching, doctors add 25-75 mg of clomipramine to a full SSRI. Research shows this boosts response rates by 35-40% in people who only partially improved on SSRIs alone. It’s like adding a second engine to a car that’s still struggling uphill.
What About the Future?
The field isn’t standing still. In March 2023, the FDA gave Breakthrough Therapy status to a new drug called SEP-363856. Early trials showed a 45% response rate in treatment-resistant OCD at just 50 mg a day. That’s huge. Meanwhile, researchers are testing psilocybin - the active ingredient in magic mushrooms - paired with SSRIs. Preliminary results show 60% of patients went into remission at six months, compared to 35% with SSRIs alone. It’s early, but promising.Even clomipramine is getting an upgrade. A new transdermal patch is in trials. Instead of swallowing a pill, you wear a patch that slowly releases the drug. Early results suggest it works just as well as 200 mg of oral clomipramine - but with 40% fewer side effects. No dry mouth. Less drowsiness. That could change everything.
Real Talk: What Patients Say
On Drugs.com, SSRIs have an average effectiveness rating of 6.8/10. Clomipramine? 7.2/10. But satisfaction? SSRIs: 6.2/10. Clomipramine: 5.1/10. The gap? Side effects. One user wrote: "Clomipramine stopped my rituals. But I felt like I was walking through molasses. I couldn’t focus at work. I quit." Another said: "I tried six SSRIs. Sertraline at 225 mg didn’t fully help, but it let me live. I’d take that over perfection any day."On OCD-UK forums, 62% of 1,247 users said SSRIs were better tolerated. Common complaints about clomipramine? "I drank 5-6 glasses of water every hour." "I gained 20 pounds and couldn’t get out of bed." But for some, those costs were worth it. "After 12 years of OCD, clomipramine at 150 mg was the first thing that gave me back my life. I’d do it again."
What to Do Next
If you’re starting treatment: expect slow progress. Don’t panic if symptoms get worse in week one. Talk to your doctor. Keep taking it. Track your symptoms weekly. Use the CY-BOCS scale if you can - even just mentally. Note how many hours your rituals take. How much do they interfere with work, sleep, relationships?If you’ve tried one SSRI and it didn’t work? Try another. Don’t give up. If two don’t work? Ask about clomipramine. Or ask about adding a low dose. If side effects are unbearable? Talk about switching. There’s no shame in changing paths.
And remember: medication isn’t the whole story. Therapy - especially exposure and response prevention (ERP) - is just as critical. The best outcomes come when pills and therapy work together. One without the other? Often not enough.
OCD doesn’t care how much you want to be free. But science does. And right now, SSRIs and clomipramine are the two best tools we have. You don’t have to find the perfect one. Just the one that lets you live.
