You’ve got a cough. It’s keeping you up at night, making you wince when you laugh, or just plain annoying. You walk into the pharmacy and stare at the wall of bottles: Robitussin, Mucinex, Delsym, NyQuil - some say "cough suppressant," others say "expectorant." What’s the difference? And why does it matter?
It matters a lot. Taking the wrong kind of OTC cough medicine won’t just waste your money - it could make you feel worse. For years, people have been popping suppressants when they needed expectorants, or vice versa, because the labels look similar and the terms sound like synonyms. But they’re not. They work in completely opposite ways.
What Does a Cough Suppressant Actually Do?
A cough suppressant, like dextromethorphan (found in Delsym, Robitussin DM, and many store brands), doesn’t treat the cause of your cough. It doesn’t clear mucus. It doesn’t fight infection. It simply tells your brain to stop triggering the cough reflex.
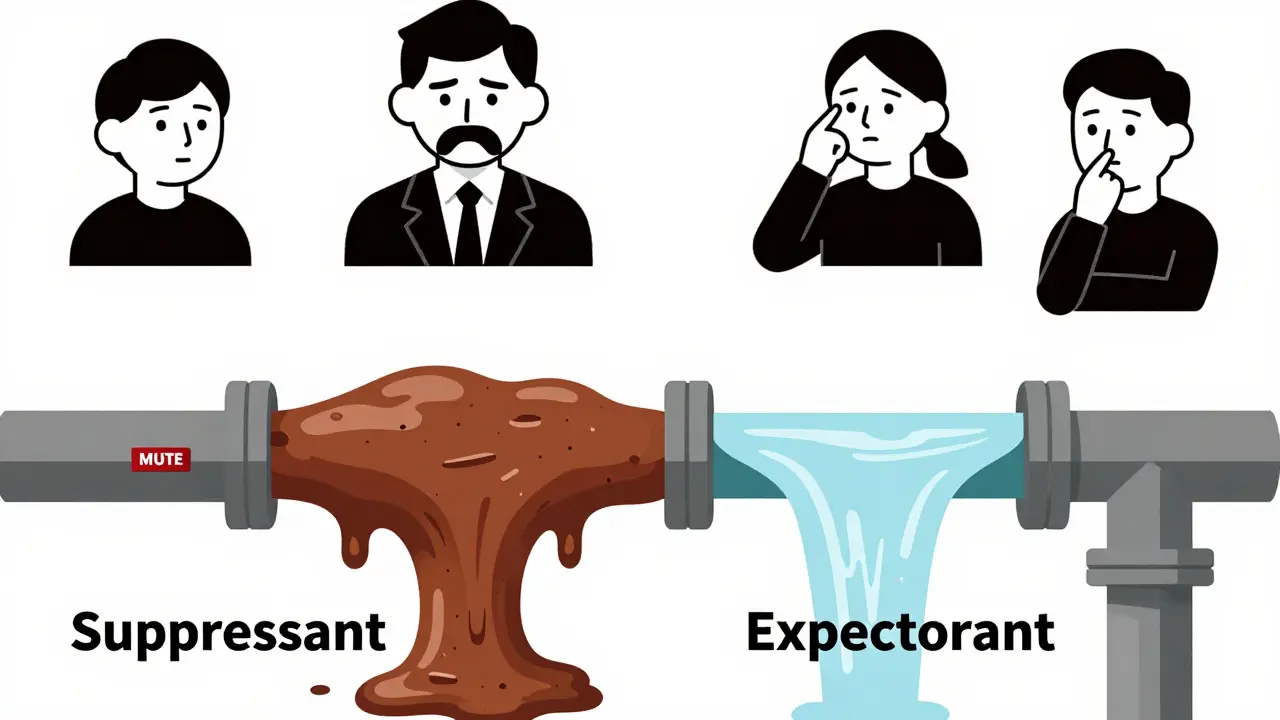
Think of your cough as an alarm system. When your airways get irritated - by smoke, dust, or post-nasal drip - your nervous system sends a signal to your brain. Your brain says, "Time to cough and clear this out." A suppressant like dextromethorphan steps in and mutes that signal. It’s like turning off the fire alarm because the noise is annoying, not because the fire is gone.
This works great for dry, hacking coughs - the kind that comes after a cold, or from throat irritation, or even from allergies. If you’re coughing so hard you’re vomiting, or you can’t sleep because your throat feels raw, a suppressant can give you relief.
But here’s the catch: if you’re coughing up phlegm - yellow, green, white, or clear - that means your body is trying to clear something out. Mucus is your body’s way of trapping viruses, bacteria, or irritants and pushing them out. Suppressing that cough is like trying to stop a leak by taping over the pipe instead of fixing the crack. You’re trapping the gunk inside, which can lead to longer illness, chest infections, or even pneumonia.
What Does an Expectorant Actually Do?
Now let’s talk about guaifenesin - the only active ingredient the FDA officially recognizes as an expectorant in OTC products. You’ll find it in Mucinex, Robitussin Chest Congestion, and many generic versions.
Unlike suppressants, expectorants don’t quiet your cough. They make it more effective. Guaifenesin works by thinning out thick, sticky mucus in your lungs and airways. It doesn’t dry you out - it hydrates you from the inside. It increases fluid in your respiratory tract, so that gunk becomes easier to cough up.
Imagine your airways are like a clogged drain. Thick mucus is like grease and hair stuck in the pipe. Guaifenesin is like pouring hot water down the drain. It loosens the gunk so your body can flush it out naturally. That’s why you’re supposed to drink a full glass of water with every dose. Without enough fluids, guaifenesin won’t work.
This is ideal for wet, productive coughs - the kind that comes with bronchitis, sinus infections, or colds that have moved into your chest. You feel congestion, you hear rattling when you breathe, and you’re coughing up mucus. That’s your body doing the right thing. Expectorants help it do it better.
Why Mixing Them Up Is a Common Mistake
Here’s where things go wrong: 43% of people who buy OTC cough medicine are using the wrong type for their symptoms, according to a 2022 Kaiser Permanente survey. Why? Because many products combine both ingredients - like Robitussin DM, which has dextromethorphan and guaifenesin.
That sounds helpful, right? "One pill for everything." But it’s not. If you have a wet cough and take a suppressant, you’re silencing your body’s natural cleanup crew. If you have a dry cough and take an expectorant, you’re stimulating mucus production when you don’t need it - which can make your cough worse.
Reddit user u/ColdSufferer2023 summed it up perfectly: "I used Robitussin DM for my phlegmy cough for 3 days before realizing I should’ve used the chest congestion version - no wonder I felt worse."
Pharmacists in the UK and US report that nearly 40% of their OTC cough medicine consultations are about people choosing the wrong product. It’s not their fault. The labels are confusing. The bottles look alike. The names are similar. And most people don’t know the difference between a dry cough and a wet cough.
How to Tell If You Have a Dry or Wet Cough
You don’t need a doctor to figure this out. Just ask yourself three simple questions:
- When you cough, do you bring up mucus? (Yes = wet cough)
- Is your throat sore and tickly, but you’re not producing anything? (Yes = dry cough)
- Is your cough worse at night, or after lying down? (That often means post-nasal drip - usually dry)
If you’re coughing up clear or white mucus, you likely have a viral infection like a cold or bronchitis. Use an expectorant. If you’re coughing hard but nothing comes out - or if you’re coughing because your throat feels irritated - go for a suppressant.
The CDC’s free online symptom checker helps 68% of users correctly identify their cough type. It takes two minutes. Use it.
What to Look for on the Label
Don’t just grab the bottle with the biggest font. Read the active ingredients.
- If you see dextromethorphan - that’s a suppressant. Use it only for dry coughs.
- If you see guaifenesin - that’s an expectorant. Use it only for wet coughs.
- If you see both - avoid unless you’re sure you need both (rare).
- Watch out for "DM" on the label - that stands for dextromethorphan and sometimes guaifenesin. It’s a combo, not a cure-all.
Also check the dosage. Dextromethorphan usually comes in 15-30 mg every 4-8 hours. Guaifenesin is typically 200-400 mg every 4 hours for immediate-release, or 600-1200 mg every 12 hours for extended-release. Don’t double up. More isn’t better.

Potential Risks and Warnings
Even "safe" OTC meds have risks.
Dextromethorphan can be misused. At high doses - way above the recommended amount - it can cause hallucinations, dizziness, and even dissociation. It’s been abused as a recreational drug, especially by teens. Stick to the label.
Guaifenesin won’t work if you’re dehydrated. You need at least 64 ounces (about 2 liters) of water a day for it to thin mucus properly. Most people drink half that. If you’re not hydrating, you’re wasting your money.
Don’t give either to children under 4. The FDA warns against it. For kids 4-6, only use if a doctor says so. And never use suppressants if your mucus is yellow or green - that’s a sign of infection. Let your body cough it out.
Also, if you’re on antidepressants - especially MAOIs - dextromethorphan can cause dangerous serotonin interactions. Talk to your pharmacist if you’re on any meds.
What’s New in 2026?
The market’s changing. In 2023, Mucinex launched "MoistureLock" - a new extended-release formula designed to keep your airways hydrated longer. It’s not magic, but it helps if you forget to drink water.
Also, the FDA is rolling out new labeling rules in 2024. Expect to see clearer icons: a "mute" symbol for suppressants, a "flush" symbol for expectorants. The goal? Cut consumer confusion by 35%.
Meanwhile, expectorant sales are growing faster than suppressants. Why? More people are learning the truth: you don’t want to silence your cough. You want to help it work better.
Bottom Line: Match the Medicine to the Symptom
Here’s your simple rule:
- Dry cough? No mucus? Throat tickles? → Use a suppressant (dextromethorphan).
- Wet cough? Mucus coming up? Chest feels heavy? → Use an expectorant (guaifenesin).
- Unclear? Wait 24-48 hours. See if mucus appears.
- Always drink water with expectorants.
- Never use suppressants if you’re coughing up colored mucus.
OTC cough medicines aren’t about getting rid of the cough. They’re about helping your body heal. The best cough medicine is the one that supports your body’s natural defenses - not fights them.
Next time you reach for a bottle, pause. Ask yourself: "Am I trying to quiet the alarm - or fix the problem?"
Can I take a cough suppressant and an expectorant together?
You can, but you shouldn’t unless you’re sure you need both. Most combination products (like Robitussin DM) contain both dextromethorphan and guaifenesin. If you have a wet cough, the suppressant could block your body’s ability to clear mucus. If you have a dry cough, the expectorant may make you produce more mucus than needed. Stick to single-ingredient products unless your pharmacist or doctor recommends otherwise.
How long should I use OTC cough medicine before seeing a doctor?
If your cough lasts more than 10 days, gets worse after a week, or is accompanied by fever, shortness of breath, chest pain, or colored mucus, see a doctor. OTC meds are for short-term relief, not long-term treatment. Persistent coughs can signal bronchitis, pneumonia, asthma, or even heart issues.
Is guaifenesin safe for people with high blood pressure?
Yes, guaifenesin is generally safe for people with high blood pressure. Unlike decongestants (like pseudoephedrine), it doesn’t raise blood pressure. But always check the full ingredient list - some Mucinex products include other active ingredients like phenylephrine or antihistamines, which can affect blood pressure. Stick to plain guaifenesin if you have hypertension.
Does dextromethorphan make you drowsy?
Yes, drowsiness is a common side effect of dextromethorphan, especially at higher doses or in sensitive individuals. Some people feel groggy, dizzy, or have trouble concentrating. Don’t drive or operate machinery until you know how it affects you. If drowsiness is a problem, try taking it at night - but only if your cough is dry and non-productive.
Why does my cough get worse at night?
Lying down causes mucus to pool in your throat and airways, triggering coughing. Post-nasal drip from allergies or sinus congestion also worsens at night. If your cough is dry and worse at night, a suppressant might help you sleep. If it’s wet, drink water before bed and prop your head up with pillows - don’t suppress the cough. Let your body clear the mucus.
If you’re still unsure, ask your pharmacist. They’re trained to help you pick the right OTC medicine - and they’re usually right there in the store. No appointment needed.
