Peritoneal dialysis lets you treat kidney failure at home - no clinic visits, no needles. But choosing between CAPD and APD isn’t just about convenience. It’s about your daily life, your sleep, your body’s response, and even your wallet.
When your kidneys fail, dialysis becomes your lifeline. Most people think of sitting in a clinic three times a week, hooked up to a machine. But for many, peritoneal dialysis at home is a better fit. It uses the lining of your belly - the peritoneum - as a natural filter. Waste and extra fluid leave your blood through a special fluid that’s swapped in and out of your abdomen. And you do it yourself. Two main ways exist: CAPD and APD. One is manual. One is automated. Neither is better for everyone. The right choice depends on your body, your routine, and your home.
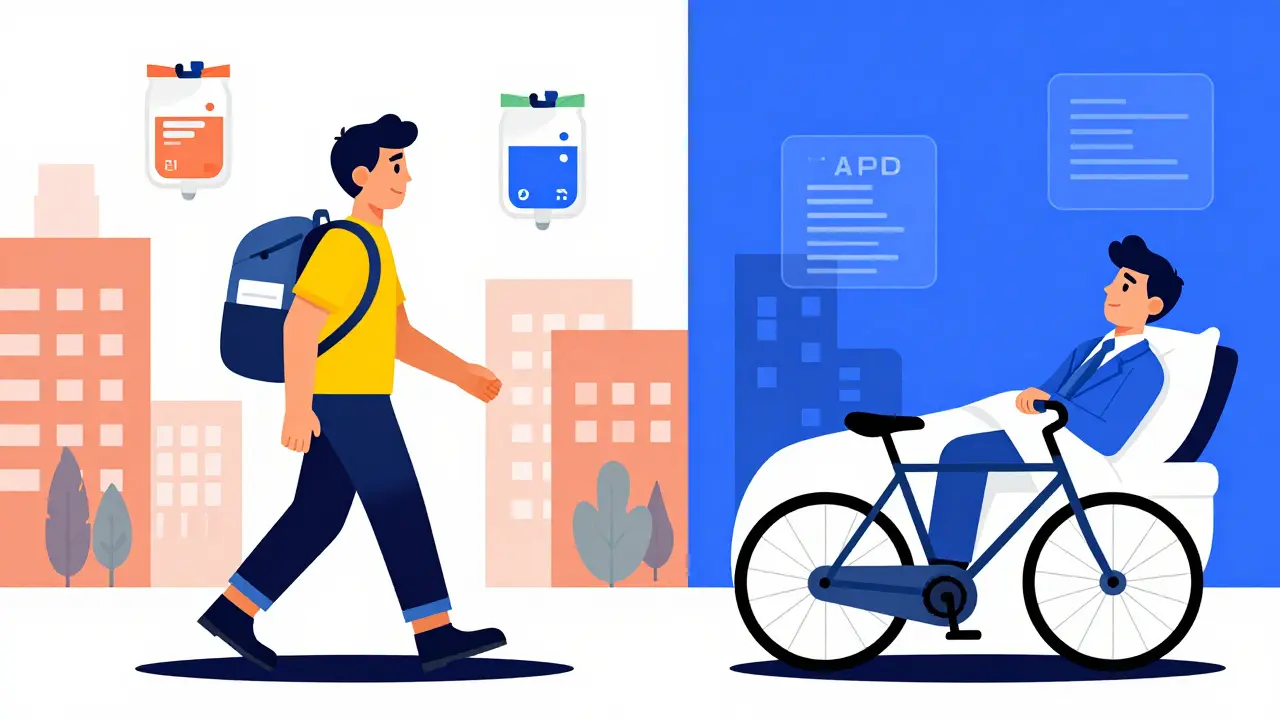
CAPD: Do It Yourself, Anytime, Anywhere
Continuous Ambulatory Peritoneal Dialysis, or CAPD, is the original home dialysis method. Developed in the 1970s, it needs no machine. You do the exchanges manually, usually 3 to 5 times a day. Each time, you connect a bag of dialysis fluid to your catheter, let gravity fill your belly, wait 4 to 6 hours, then drain it out. Each exchange takes about 30 to 40 minutes. You can do it while sitting, standing, or even walking.
That’s the big sell: freedom. You’re not tied to a machine. You can travel, work, or run errands without planning around a nightly cycle. Many people who do CAPD keep full-time jobs. A 2023 Kidney.org report found 65% of CAPD users are employed - higher than those on APD. If you hate being tethered to one spot, CAPD gives you mobility. You carry your fluid bags in a small backpack. Each bag weighs about 1.5 to 3 kilograms. You stash extras in your closet or fridge. No electricity needed. No setup. Just clean hands, clean space, and steady technique.
But here’s the catch: your days get broken up. Every 4 to 6 hours, you stop what you’re doing to swap fluid. For teachers, nurses, or parents, that means scheduling around meals, meetings, or bedtime routines. And if you’re not careful with sterile technique, you risk peritonitis - a serious belly infection. USRDS data shows CAPD users have 0.68 infections per year on average, higher than APD’s 0.52. That’s not a huge gap, but it adds up over time. And if you have arthritis, shaky hands, or trouble bending, CAPD can be physically tough. About 38% of dialysis patients over 65 struggle with manual dexterity. For them, CAPD becomes a chore, not a cure.
APD: Let the Machine Work While You Sleep
Automated Peritoneal Dialysis, or APD, uses a machine - a cycler - to do the exchanges for you, overnight. You connect to the device before bed, and while you sleep, it fills and drains your belly automatically, usually 8 to 10 times over 8 to 10 hours. The machines, like the Baxter Amia or Fresenius Sleep-Safe, are about the size of a small suitcase, weigh 15 to 25 pounds, and need a power outlet. You set them up once, and they handle the rest.
The biggest advantage? Your days are uninterrupted. No midday exchanges. No carrying bags. You wake up with your treatment done. That’s why APD is popular among working adults. Mayo Clinic data from 2022 shows APD users get an extra 3.2 hours of sleep per night compared to CAPD users. That’s not just comfort - it’s better mental health, sharper focus, and more energy for daily life.
APD also offers better fluid control. A 2021 meta-analysis in Nephrology Dialysis Transplantation found APD users had 22% fewer episodes of dangerous fluid overload - a major cause of hospital visits. Better fluid balance means lower blood pressure, less swelling, and fewer heart stresses. That’s why Medicare data shows APD users have 18% fewer hospitalizations for fluid-related issues.
But APD isn’t perfect. You need reliable electricity. A power outage? You’re stuck. Cyclers can break. About 12% of users experience a machine malfunction each year. When that happens, you need to switch to manual exchanges - and not everyone knows how. You also need space: a flat surface for the machine, room to store supplies, and quiet enough for sleep. Cyclers make about 35 to 45 decibels of noise - like a library. For light sleepers, that’s a problem. Some users report discontinuing APD because the noise keeps them awake.

Cost, Training, and Support: What’s Really Involved
Cost isn’t just about the machine. In the U.S., Medicare covers 80% of home dialysis. But out-of-pocket costs vary. CAPD supplies cost $50 to $75 a month. APD? $75 to $100, because you’re renting the cycler. Some insurance plans cover the rental, but not all. Long-term, APD might save you money - better fluid control means fewer meds for high blood pressure and phosphorus, cutting costs by 15-20% over time, according to USRDS data from 2021.
Training is longer for APD. CAPD takes 10 to 14 days. You learn sterile technique, how to connect bags, and how to spot infection signs. APD takes 14 to 21 days. You learn machine operation, error codes, backup procedures, and how to handle a breakdown. Both require a clean, dedicated space - about 4x4 feet for supplies. APD adds the need for an outlet and a quiet corner for the machine.
Support differs, too. Fresenius reports 95% of APD programs offer 24/7 technical help for machine issues. Only 82% of CAPD programs offer the same for clinical questions. And here’s something new: 78% of APD systems now include remote monitoring. Your cycler sends data - fluid volume, dwell times, pressure readings - directly to your care team. If something’s off, they call you before you get sick. That cuts emergency visits by 25%, according to Kidney International Reports (2022). CAPD has no such tech. You’re on your own until symptoms show up.
Who Benefits Most From Each?
There’s no one-size-fits-all. But patterns emerge.
CAPD is often better for:
- People over 75 - simpler, no machine to manage
- Those with limited home space - no bulky equipment
- Travelers or people on the move - no power needed
- Patients with good manual dexterity and steady routines
- Those in areas with unreliable electricity
APD is often better for:
- Working adults under 65 - no daytime interruptions
- People who struggle with sleep quality on CAPD
- Those with high blood pressure or fluid overload issues
- Patients with dexterity problems - the machine does the work
- People with reliable power and space for a machine
Dr. Michael J. Germain, a nephrologist at Baystate Medical Center, says CAPD remains the gold standard for patients over 75 because it’s cognitively simpler. Dr. Beth Piraino from UPMC argues that for anyone under 65, APD should be the first option - modern cyclers are so reliable, the barrier is gone.
But here’s the reality: it’s not just medical. It’s personal. A CAPD user on Reddit said: “I exchange during my lunch break. I feel in control.” An APD user wrote: “I sleep through my treatment. I don’t think about it until morning.” One isn’t right. Both can be right - for different people.
The Future: Tech Is Changing the Game
APD is growing fast. GlobalData reports APD adoption is rising at 7.3% a year - triple the rate of CAPD. Why? Better tech. Baxter’s Amia system, launched in 2021, uses AI to adjust fluid removal based on your weight and blood pressure. In trials, it cut fluid overload events by 31%. New cyclers are quieter, smaller, and can be controlled by smartphone apps. The FDA is expected to clear the first smartphone-connected cycler in 2025 - it could reduce setup errors by 40%.
Meanwhile, CAPD isn’t disappearing. It’s still vital in rural areas, low-income communities, and countries without advanced healthcare systems. In the U.S., only 32% of rural clinics offer full home dialysis training. CAPD doesn’t need tech - just a trained nurse and clean hands.
By 2030, APD will make up 65% of home peritoneal dialysis, according to the Global Dialysis Outlook. By 2035, it may be the default. But CAPD will still matter - for the elderly, the resource-limited, and those who prefer doing things themselves.
What Should You Do?
Don’t pick based on what’s trendy. Pick based on your life.
Ask yourself:
- Can I do a sterile exchange 4 times a day without help?
- Do I have a quiet, safe space for a machine at night?
- Is my power reliable? What if the electricity goes out?
- Do I travel often? Can I carry fluid bags easily?
- Do I have arthritis, tremors, or vision problems?
- Am I okay with being woken up if the machine fails?
Talk to your nephrologist. Ask for a trial. Some clinics let you try CAPD for a week, then APD for a week. See how your body reacts. See how your schedule holds up.
Remember: survival rates are nearly the same for both. Five-year survival is 52-58% for home PD - better than clinic hemodialysis. The goal isn’t just to live longer. It’s to live better. To sleep through the night. To work your job. To take your grandkids to the park. To not be defined by your treatment.
Peritoneal dialysis at home isn’t a compromise. It’s a choice. And the right one isn’t about the machine. It’s about the life you want to live.
Can I switch from CAPD to APD later if I change my mind?
Yes, you can switch between CAPD and APD at any time, as long as your catheter is working and your health is stable. Many people start with CAPD to get used to home dialysis, then switch to APD once they’re comfortable. Others begin with APD and switch to CAPD if they lose power often or find the machine too noisy. Your care team will guide you through the transition - it’s not a one-way decision.
Is one method safer than the other?
Both are safe when done correctly, but they carry different risks. CAPD has a slightly higher risk of peritonitis because you handle the lines and bags manually. APD reduces that risk by automating the process, but introduces machine-related risks - like malfunctions or power outages. The overall infection rate is low for both, and modern training programs cut risks by more than half. The key is training and consistency - not which method you pick.
What if I live in a small apartment or don’t have space for a machine?
CAPD is your best option. It requires no machine, just a clean surface to lay out your supplies - a kitchen counter or bedside table works. APD needs space for the cycler, storage for bags, and an outlet. If your home is tight, CAPD gives you flexibility. Some people store supplies under the bed or in a closet. A 4x4 foot area is enough. If you’re unsure, ask your home dialysis nurse to do a home assessment before you decide.
Do I need a caregiver to help me with either method?
Not necessarily. Many people do both CAPD and APD alone. But having a caregiver helps - especially at first. Medicare now covers training for family members as care partners (2024 rule change). If you have tremors, vision problems, or memory issues, a helper is a good idea. APD users benefit from someone who can check the machine if it alarms. CAPD users may need help with bag changes if they can’t bend or reach. You don’t need a full-time caregiver, but having someone nearby for emergencies makes things safer.
How do I know if I’m a good candidate for home dialysis at all?
Most people with kidney failure are candidates - if they’re motivated and have support. Your doctor will check your heart health, abdominal anatomy (to make sure your peritoneum works well), and mental health. You need to be able to follow instructions and handle basic hygiene. You don’t need to be perfect - just consistent. About 23% of people who start home dialysis need minor home modifications - like a handrail or better lighting. If you’re willing to make those small changes, you’re likely a good fit.
