When your urine looks foamy or bubbly for days on end, it’s not just about what you ate. It could be your kidneys sending out a warning signal. That signal is proteinuria - too much protein leaking into your urine. It’s not a disease on its own, but it’s one of the clearest early signs your kidneys are struggling. And if you ignore it, the damage can get worse - fast.
What Exactly Is Proteinuria?
Your kidneys are like high-tech filters. They keep proteins - the building blocks of muscle, skin, and immune function - in your blood where they belong. Healthy kidneys let through less than 150 milligrams of protein per day. Most of that is invisible. But when the filters break down, protein escapes. Albumin, the most common protein found in urine, is the red flag doctors look for. That’s why proteinuria is often called albuminuria.
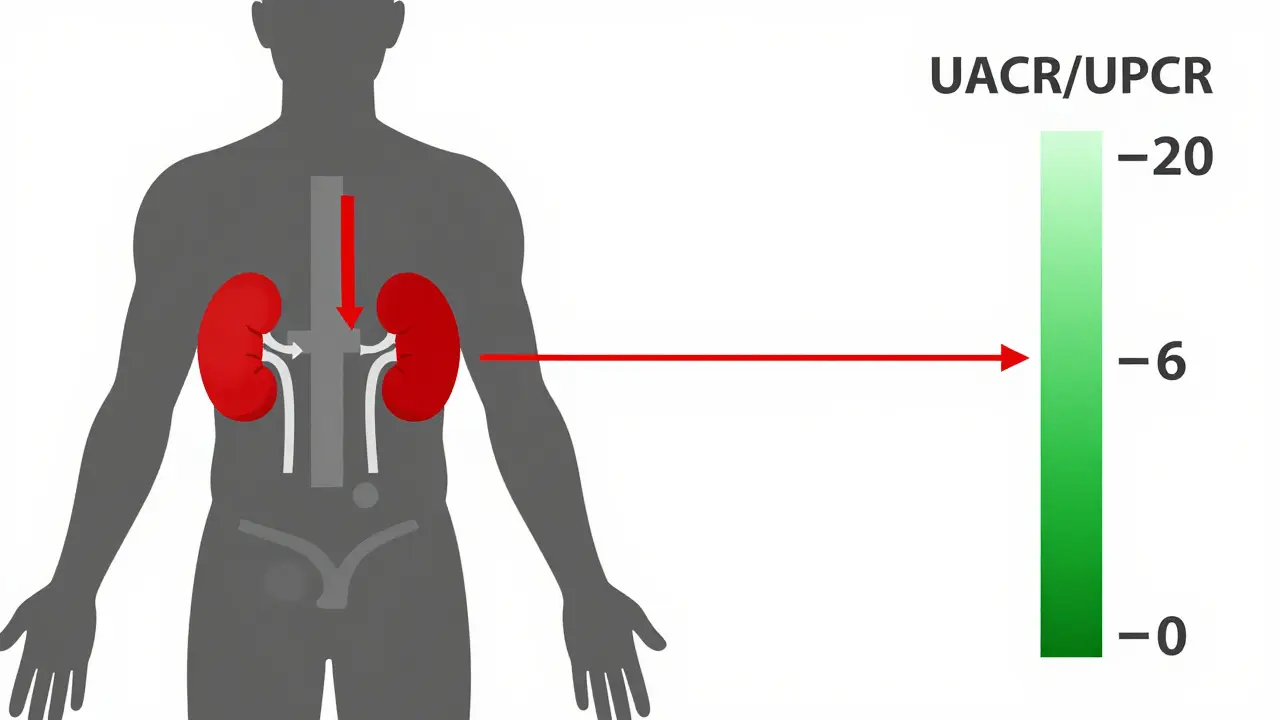
It’s not always serious. Sometimes, stress, a fever, or a hard workout can cause a temporary spike. But if protein keeps showing up over weeks or months, it’s a sign your kidneys are under pressure. The UK’s NICE guidelines say proteinuria becomes a concern when your urine protein-to-creatinine ratio (UPCR) hits 45 mg/mmol or higher. For most people, anything over 30 mg/mmol in urine albumin-to-creatinine ratio (UACR) needs checking.
How Do You Know You Have It?
The scary part? Most people feel nothing at first. Up to 70% of those with mild proteinuria have no symptoms. That’s why routine testing matters - especially if you’re diabetic, hypertensive, or over 50.
When protein levels climb above 1,000 mg per day, symptoms start to show:
- Foamy or bubbly urine - the most common sign, seen in 85% of people with noticeable proteinuria
- Swelling in ankles, feet, hands, or face - caused by low protein levels in the blood pulling fluid out of vessels
- Feeling tired all the time, even after rest
- More frequent urination, especially at night
- Nausea, loss of appetite, or muscle cramps
If you’re losing more than 3,500 mg of protein daily, you might be developing nephrotic syndrome - a serious condition that also brings high cholesterol and severe swelling. This needs urgent care.
How Is It Diagnosed?
Doctors don’t guess. They test.
The first step is usually a dipstick test - a quick paper strip dipped in your urine sample. It gives a rough idea: trace, small, moderate, or large. But it’s not accurate enough on its own. False negatives are common, especially with early-stage proteinuria.
The real answer comes from two tests:
- Spot UPCR or UACR: A single urine sample tested for protein or albumin compared to creatinine. This is now the standard in the UK and US. A UACR over 30 mg/g means proteinuria. Over 300 mg/g is severe.
- 24-hour urine collection: You collect every drop of urine for a full day. It’s accurate but messy. Many people forget or skip it. That’s why spot tests are preferred - they’re 95% as reliable when done right.
In complex cases, doctors may run an electrophoresis test to see exactly which proteins are leaking. That helps spot rare causes like multiple myeloma, where abnormal proteins called Bence-Jones show up.
What’s Causing It?
Not all proteinuria is the same. The cause changes how you treat it.
Transient proteinuria - temporary and harmless - affects about 25% of healthy adults. Triggers include:
- Dehydration (18% of cases)
- Intense exercise (15%)
- Fever or infection (12%)
- Emotional stress (8%)
- Extreme cold or heat (5%)
Once the trigger is gone, so is the protein.
Persistent proteinuria is the real concern. It’s linked to chronic conditions:
- Diabetic nephropathy - 40% of cases
- High blood pressure - 25%
- Glomerulonephritis (kidney inflammation) - 15%
- Lupus or other autoimmune diseases - 7%
- Preeclampsia during pregnancy - 5%
- Heart disease, amyloidosis, or multiple myeloma - 8% combined
If you have diabetes or high blood pressure, proteinuria isn’t just a symptom - it’s proof your kidneys are already being damaged. And the more protein you lose, the faster the damage progresses. Studies show people losing over 1 gram of protein daily have a 50% chance of reaching kidney failure within 10 years - if nothing changes.
How to Reduce Proteinuria and Protect Your Kidneys
Good news: you can slow or even reverse early kidney damage. It’s not about magic pills. It’s about consistent, smart choices.
1. Control Your Blood Pressure
Keeping your blood pressure under 130/80 mmHg is one of the most powerful tools. Every 10 mmHg drop in systolic pressure can cut protein loss by 20-40%. ACE inhibitors (like lisinopril) and ARBs (like losartan) are first-line treatments. They don’t just lower pressure - they directly protect the kidney filters. Studies show they reduce proteinuria by 30-50%.
Side effect? A dry cough in about 40% of users. If that happens, your doctor can switch you to an ARB - same benefit, less cough.
2. Manage Blood Sugar (If You’re Diabetic)
High blood sugar is the #1 cause of kidney damage. Tight control matters. But now, newer drugs are changing the game. SGLT2 inhibitors - like canagliflozin or dapagliflozin - were originally for diabetes. Now we know they cut proteinuria by 30-40% and slow kidney decline by 30%. They’re now recommended for diabetics with proteinuria, even if blood sugar is under control.
3. Try Finerenone
For people with type 2 diabetes and kidney disease, a new drug called finerenone has shown promise. In the FIDELIO-DKD trial, it reduced proteinuria by 32% and cut the risk of kidney failure by 18%. It’s not for everyone, but if you’re on ACE/ARB and still leaking protein, ask your doctor about it.
4. Adjust Your Diet
Protein restriction sounds counterintuitive - but it helps. Eating too much protein forces your kidneys to work harder. Experts recommend 0.6-0.8 grams of protein per kilogram of body weight per day. For a 70kg person, that’s 42-56 grams daily - about the amount in 2 eggs, 100g chicken, and a cup of lentils.
Work with a renal dietitian. Too little protein can cause muscle loss. Too much speeds up damage. Balance is everything. Also, cut back on salt. Sodium worsens swelling and raises blood pressure.
5. Monitor and Follow Up
Testing isn’t a one-time thing. If you’ve been diagnosed:
- Check UPCR every 3-6 months if stable
- Check monthly when starting new meds
- Target at least a 30% drop in proteinuria within 3 months
Studies show that every 50% reduction in proteinuria lowers your risk of kidney failure by 30%. That’s huge.
What’s New in Testing and Treatment?
Technology is catching up. Smartphone apps that analyze urine color and foaminess are now hitting 85% accuracy compared to lab tests. They’re not replacements - but they’re great for tracking changes at home.
Researchers are also finding new biomarkers. Urinary TNF receptor-1 levels now predict which patients will decline fastest. Genetic testing is helping identify rare inherited conditions like Alport syndrome - where a new drug, bardoxolone methyl, reduced proteinuria by 35% in trials.
The global market for proteinuria tests is set to hit $2.1 billion by 2027. Why? Because we’re getting better at catching it early - and treating it before it’s too late.
Who Should Be Tested?
You don’t need to wait for symptoms. If you fall into any of these groups, get tested yearly:
- People with type 1 or type 2 diabetes
- Those with high blood pressure
- People with heart disease or obesity
- Anyone with a family history of kidney disease
- Adults over 60
Even if you feel fine. Kidneys don’t complain until they’re nearly broken.
Final Thoughts: Catch It Early, Act Fast
Proteinuria isn’t a death sentence. It’s a warning light. And like any warning light, the sooner you respond, the better your outcome.
Most people who catch it early - and stick to treatment - never need dialysis. They live full lives. But if you ignore it, the damage is often irreversible.
Don’t wait for swelling or foamy urine to show up. If you’re at risk, ask your GP for a simple urine test. It takes five minutes. It could save your kidneys - and your future.
Is foamy urine always a sign of kidney problems?
Not always. Foamy urine can happen after a hard workout, when you’re dehydrated, or even from fast urination. But if it’s persistent - happening daily for more than a week - it’s a red flag. Test it. Don’t assume it’s harmless.
Can I test for proteinuria at home?
Yes, but with limits. Over-the-counter dipstick tests are available, but they’re not as accurate as lab tests. New smartphone apps that analyze urine foam are promising, with 85% accuracy. They’re great for tracking changes over time, but never replace a doctor’s UPCR test for diagnosis.
Does cutting protein in my diet help reduce proteinuria?
Yes - but only if you do it right. Eating too much protein stresses damaged kidneys. Reducing intake to 0.6-0.8g per kg of body weight can lower protein loss by 15-25%. But going too low can cause muscle wasting. Always work with a renal dietitian to find your safe range.
Are ACE inhibitors the best treatment for proteinuria?
They’re still first-line - especially for diabetics and hypertensives. ACE inhibitors and ARBs reduce proteinuria by 30-50% and slow kidney decline. But newer drugs like SGLT2 inhibitors and finerenone are now used alongside them for even better results. Treatment is often layered, not one-size-fits-all.
Can proteinuria be reversed?
In early stages - yes. If caught before scarring sets in, reducing proteinuria through medication, blood pressure control, and diet can allow the kidney filters to heal partially. But once significant scarring occurs, the damage is permanent. The goal shifts from reversal to slowing further loss.
How often should I get my urine tested if I have diabetes?
Annually, at minimum. If you already have proteinuria, test every 3-6 months. If you’re starting new treatment, test monthly for the first 3-6 months to track response. The American Kidney Fund and NICE both recommend this for diabetics - it’s not optional, it’s essential.
Does alcohol or smoking affect proteinuria?
Yes. Smoking damages blood vessels, including those in the kidneys, and speeds up protein leakage. Alcohol can raise blood pressure and worsen dehydration - both increase proteinuria. Quitting smoking and limiting alcohol are critical parts of kidney protection.
Next Steps: What to Do Today
If you’re at risk - diabetic, hypertensive, over 50, or just concerned - take action now:
- Ask your GP for a urine UACR or UPCR test. It’s cheap, fast, and covered by the NHS.
- If you’re on blood pressure meds, make sure they’re ACE inhibitors or ARBs - not just any pill.
- Start tracking your weight daily. Sudden gain (2kg in 2 days) means fluid buildup - a sign proteinuria is worsening.
- Download a simple urine foam tracker app. Use it to log changes between visits.
- Set a reminder: annual kidney check, no exceptions.
Your kidneys don’t shout. They whisper. Listen before it’s too late.