When you’re on a proton pump inhibitor (PPI) like omeprazole for heartburn and suddenly need an antifungal for a serious infection, something unexpected can happen: the antifungal stops working as well as it should. This isn’t a myth or a guess-it’s a well-documented, clinically significant interaction that affects thousands of patients every year. The problem? PPIs raise the pH in your stomach, and that change kills the absorption of certain antifungal drugs. If you’re taking itraconazole capsules, posaconazole tablets, or even voriconazole with a PPI, you might not be getting enough of the drug into your bloodstream to fight the fungus. And if you don’t know this, your infection could get worse-maybe even become deadly.
Why Your Stomach Acid Matters for Antifungals
Most people think stomach acid is just there to digest food. But for some antifungal medications, it’s the key to getting into your system. Drugs like itraconazole and posaconazole are weak bases. That means they need a low pH-around 3 or lower-to dissolve properly. Without enough acid, these pills just sit in your stomach like little rocks, never breaking down enough to be absorbed. PPIs shut down your stomach’s acid pumps entirely. Instead of a pH of 1-2, your stomach might hover at 4-6. That’s enough to cut the absorption of itraconazole by up to 60%, according to JAMA Network Open (2023). That’s not a small drop. That’s the difference between a therapeutic dose and a useless one.Not All Antifungals Are Affected the Same Way
This isn’t a blanket rule. Some antifungals don’t care about stomach pH at all. Fluconazole, for example, dissolves easily in water and gets absorbed no matter how acidic your stomach is. Studies show its levels stay steady whether you’re on omeprazole or not. Voriconazole? It’s in the middle. It loses about 22-35% of its absorption with PPIs, depending on the formulation. But itraconazole capsules? They’re the most vulnerable. The FDA labeling from 1996 first flagged this, and since then, dozens of studies have confirmed it. The same goes for posaconazole delayed-release tablets. If you’re on one of these, and you’re also on a PPI, you’re at risk.The Solution Isn’t One-Size-Fits-All
You can’t just stop your PPI. If you’re on it for a bleeding ulcer or severe GERD, turning it off could be dangerous. So what do you do? First, know your formulation. Itraconazole comes in two forms: capsules and solution. The capsules need acid. The solution? It’s already dissolved. Studies show the solution only drops 10-15% in absorption with PPIs-not enough to matter. Switching from capsules to solution can fix the problem without ditching your acid control. For posaconazole, the oral suspension is better than the tablet if you’re on a PPI. And if you must use the tablet, try taking it with a cola drink. The acidity helps. One study showed it boosted absorption by 35%.Timing Matters-But Only Sometimes
Some doctors tell you to space out the doses. Take the antifungal two hours before the PPI. That works for the itraconazole solution. But for capsules? Even spacing doesn’t help much. The PPI’s effect lasts 12-24 hours. By the time you take the capsule, your stomach is still too basic. H2 blockers like famotidine are a better alternative. They don’t raise pH as high or as long. One study found famotidine reduced itraconazole absorption by only 41%, compared to 57% with omeprazole. If you need acid suppression and you’re on itraconazole capsules, famotidine taken 10 hours after the antifungal might be your best bet.
Therapeutic Drug Monitoring Is Non-Negotiable
If you’re on itraconazole for invasive aspergillosis or coccidioidomycosis, you need to know your blood levels. The target range is 0.5 to 1.0 mcg/mL. If you’re below that, you’re not protected. Many hospitals now routinely check these levels. A 2022 survey of 1,247 hospital pharmacists found 68% saw at least one case a month where PPIs caused subtherapeutic levels. One pharmacist in Massachusetts General Hospital documented a patient whose itraconazole level jumped from 0.3 to 1.7 mcg/mL after switching from omeprazole to famotidine. That’s the kind of change that saves lives. Don’t assume the pill is working. Test it.The Surprising Twist: PPIs Might Help-In the Lab
Here’s the weird part. In test tubes, omeprazole and itraconazole together kill fungus better than either drug alone. A 2025 study in Frontiers in Pharmacology found this synergy worked against 77.6% of fungal strains, including drug-resistant Aspergillus fumigatus. It’s not clear why yet. Maybe the PPI changes the fungal cell membrane. Maybe it blocks a resistance pathway. Either way, researchers at the NIH are now running a phase I trial (NCT05678901) to see if low-dose omeprazole can boost weak itraconazole doses in resistant infections. This isn’t something you should try at home. But it’s a sign that this interaction isn’t just a problem-it might be a clue to a new treatment.New Formulations Are Changing the Game
In 2023, the FDA approved a new version of itraconazole called Tolsura. It’s designed to absorb regardless of stomach pH. In trials, it showed only an 8% drop in absorption with PPIs-compared to 50% for the old capsules. That’s huge. If you’re on a PPI and need itraconazole, ask your doctor if Tolsura is an option. It’s more expensive, but if you’re avoiding treatment failure, it might be worth it.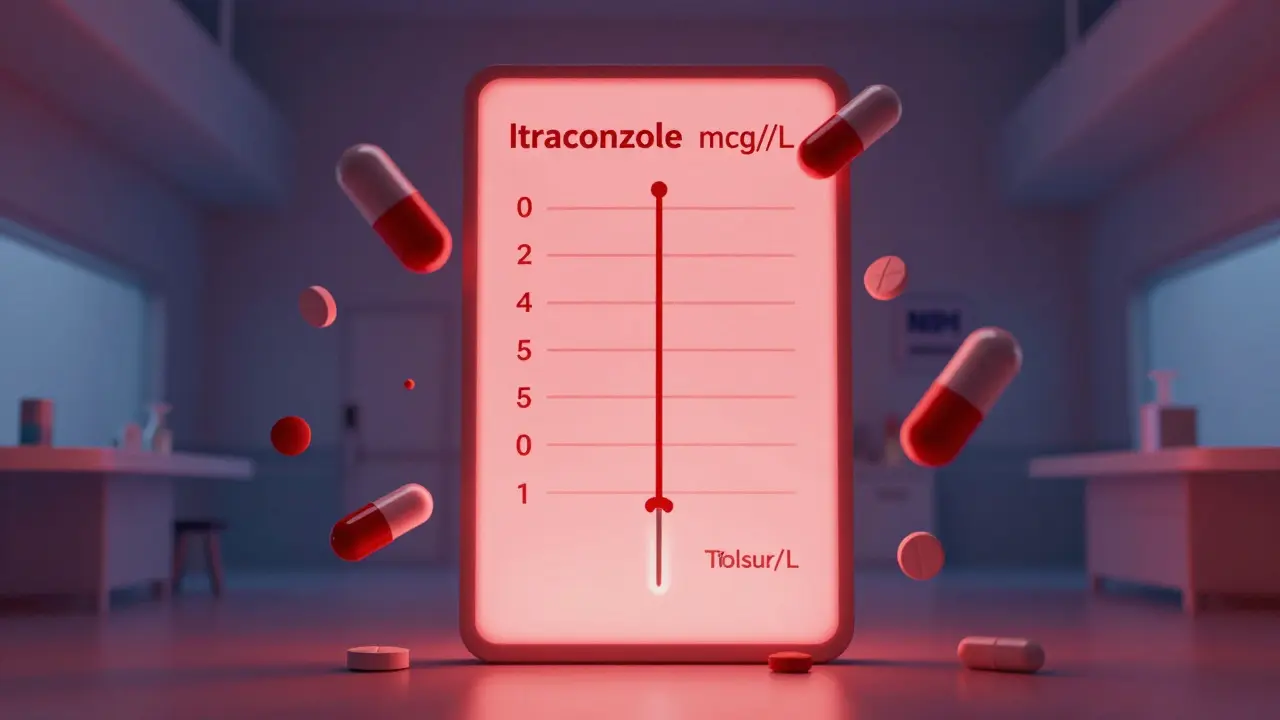
Who’s at Risk? And How Often Does This Happen?
About 15% of U.S. adults take PPIs long-term. In hospitals, 20-30% of patients on antifungals are also on PPIs. That’s a massive overlap. Medicare data from 2022 showed 38.7% of patients prescribed itraconazole capsules also got a PPI in the same month. Only 12.3% of those on the solution did. That tells you something: many providers still don’t know the difference. The cost? Around $287 million a year in wasted drugs and extra treatments for failed infections, according to JAMA Internal Medicine (2021). This isn’t rare. It’s routine-and preventable.What Should You Do Right Now?
If you’re on a PPI and prescribed an antifungal:- Check which antifungal you’re getting. Is it itraconazole capsules? Posaconazole tablets? Those are red flags.
- Ask if there’s an alternative: fluconazole (no interaction), itraconazole solution, or Tolsura.
- If you must use a PPI, ask about switching to famotidine.
- Ask if therapeutic drug monitoring is available for your antifungal.
- Don’t take antifungals with antacids unless you space them 2 hours apart.
And if you’re a clinician: don’t assume. Ask. Check. Monitor. This interaction is listed in every drug database. But in the rush of a hospital shift, it’s easy to miss. A 2023 study showed that when pharmacists intervened, 82% of patients got the right management. That’s the power of a second pair of eyes.
What’s Coming Next?
The American Gastroenterological Association and IDSA are working on updated guidelines expected by the end of 2024. They’ll have to balance two things: preventing fungal treatment failure and avoiding unnecessary PPI withdrawal in high-risk patients. One thing’s clear: blanket advice like “stop all PPIs” is outdated. The future is personalized: know the drug, know the patient, know the levels.Can I take fluconazole with a proton pump inhibitor?
Yes. Fluconazole is not affected by stomach pH changes. It dissolves easily in water and absorbs just as well whether you’re on omeprazole, pantoprazole, or nothing at all. It’s often the preferred antifungal when patients need acid suppression.
Why does itraconazole capsule fail with PPIs but the solution doesn’t?
Itraconazole capsules rely on stomach acid to dissolve the drug so it can be absorbed. PPIs raise stomach pH, preventing dissolution. The solution is already dissolved in liquid, so it doesn’t need acid to break down. It absorbs directly through the gut lining.
Should I stop my PPI if I need itraconazole?
Not always. If you’re at high risk for GI bleeding or have severe GERD, stopping your PPI could be dangerous. Instead, switch to itraconazole solution, use Tolsura, or replace the PPI with famotidine. Always talk to your doctor-don’t stop on your own.
Is there a test to check if my antifungal is working?
Yes. For itraconazole, a blood test called therapeutic drug monitoring measures your trough levels. The goal is 0.5-1.0 mcg/mL. If you’re below that, your dose may be too low or your PPI is interfering. This test is standard in hospitals treating invasive fungal infections.
Can I take antacids with antifungals if I’m on a PPI?
Antacids cause a short, sharp rise in pH, but their effect fades in 1-2 hours. If you take an antacid at least 2 hours before or after your antifungal, it usually won’t interfere. But don’t rely on this if you’re on a PPI-the PPI’s effect lasts much longer and is the bigger problem.
Are there new antifungals that don’t interact with PPIs?
Tolsura, a new formulation of itraconazole approved in 2023, is designed for pH-independent absorption. It only drops 8% in effectiveness with PPIs, compared to 50% for older capsules. Voriconazole and isavuconazole also have less pH dependence than itraconazole capsules.