When you pick up a prescription, do you ever check the label to see if it’s the brand name or the generic? For most people, it doesn’t matter-until it does. A patient might switch from Lipitor to atorvastatin and suddenly feel like something’s off. Their cholesterol hasn’t changed, but they swear the generic doesn’t work the same. Why? It’s not the chemistry. It’s the brand psychology.
Why Patients Doubt Generics, Even When They Work
Generic drugs contain the exact same active ingredients as their brand-name counterparts. They’re held to the same FDA and EMA standards. Bioequivalence is measured within an 80-125% confidence range-meaning the body absorbs them almost identically. So why do nearly 25% of patients on statins believe their generic version is less effective? It’s not about science. It’s about expectation. Studies show patients who’ve used a brand-name drug for years develop a mental association between the pill’s shape, color, and packaging, and how they feel after taking it. When that changes-even if the drug inside is identical-the brain interprets the difference as a loss of efficacy. This is called the placebo effect in reverse. The mind expects less, so the body responds with less. One 2024 study in Nature Communications found that 72% of patients reported dissatisfaction with at least one generic medication. But here’s the twist: when researchers asked them to rate effectiveness blind-without knowing which was generic or brand-the difference vanished. The pills were the same. The perception wasn’t.What Actually Drives Patient Satisfaction
Researchers have built tools to measure this. The Generic Drug Satisfaction Questionnaire (GDSQ) is one of the most validated. It breaks satisfaction into three parts: effectiveness, convenience, and side effects. Each is scored separately. Effectiveness? That’s the big one. Patients rate it based on how they feel-energy levels, symptom control, mood. Not lab results. A person taking levothyroxine might see their TSH levels are perfect, but if they still feel tired, they’ll say the generic didn’t work. Convenience matters more than you think. If a patient used to get a blue oval pill and now gets a white round one, they might forget to take it. Or they’ll think the change means something’s wrong. A 2023 study showed patients who switched to generics with unfamiliar packaging were 31% more likely to miss doses. Side effects? Often, they’re not new. They’re remembered. A patient who had mild nausea on brand-name medication might blame the generic for the same feeling-even if it’s just stress or a virus.The Role of the Doctor-and the Pharmacist
The biggest predictor of patient satisfaction with generics? What their doctor says. A 2024 study in Frontiers in Pharmacology found that when a physician explained bioequivalence clearly-using simple language like “This is the same medicine, just cheaper”-patient satisfaction jumped by 41%. When they didn’t, satisfaction dropped by 29%. Pharmacists matter too. In the UK, where pharmacists routinely counsel patients on substitutions, generic acceptance rates are 18% higher than in the U.S. Why? Because patients feel informed, not replaced. One patient on Reddit wrote: “My doctor just said ‘it’s the same.’ I didn’t believe him. Then my pharmacist sat down and showed me the FDA paperwork. That’s when I trusted it.”Some Drugs Are Trickier Than Others
Not all generics are treated the same. Antibiotics? Almost no complaints. Patients take them for a week and get better. No mystery. But drugs for epilepsy, thyroid conditions, or mental health? That’s where the anxiety spikes. Take levothyroxine. The difference between 100mcg and 105mcg can throw someone into hyper- or hypothyroidism. Even though generics are bioequivalent, tiny variations in fillers or absorption rates can matter for people who are extremely sensitive. That’s why some endocrinologists still prescribe brand-name Synthroid-even though it costs 10x more. Antidepressants are another hotspot. A 2023 survey in the Journal of Generic Medicines found that 32% of negative comments about generics came from people on SSRIs. One user wrote: “I was stable on Celexa for five years. Switched to citalopram. Felt like I was falling apart. Went back to brand. Instantly better.” Was it the drug? Maybe. But more likely, the stress of switching triggered a relapse. The mind doesn’t distinguish between chemical and psychological change.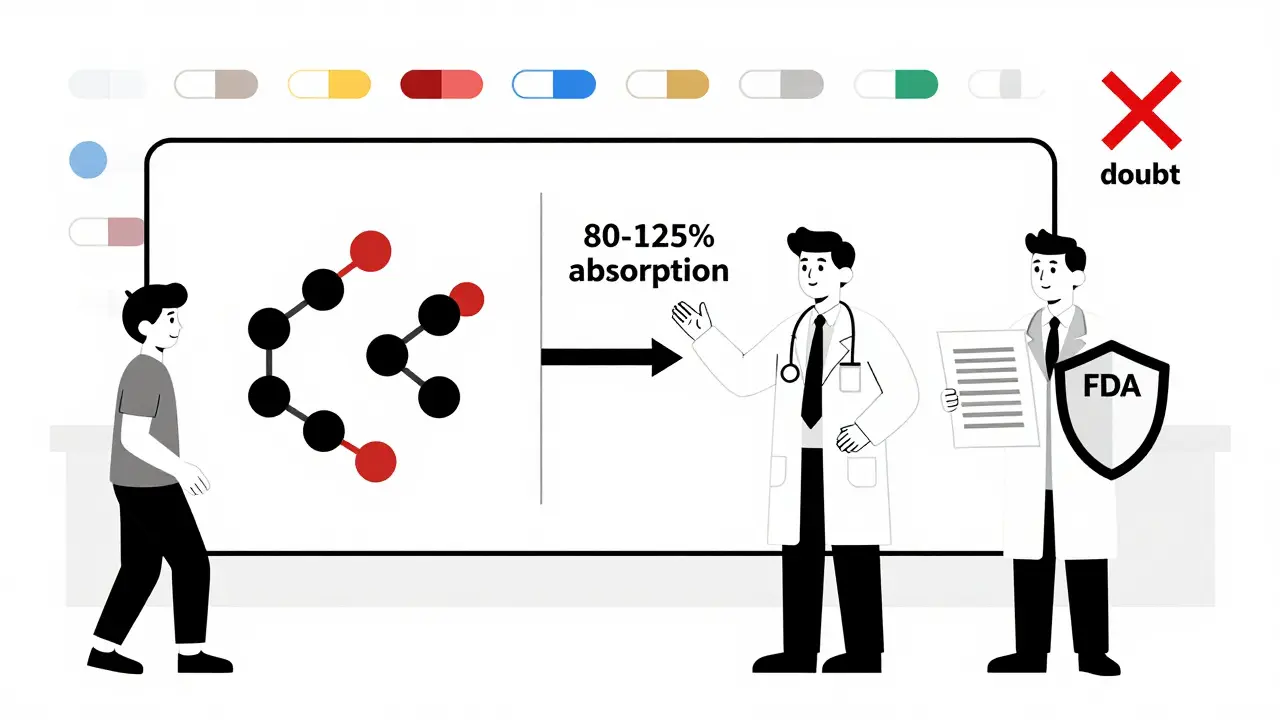
Cost Isn’t Just Money-It’s Peace of Mind
Here’s the irony: patients who care most about cost are often the most satisfied with generics. In Saudi Arabia, 64% of patients said the lower price let them take their meds consistently. In the U.S., low-income patients on insulin or blood pressure meds report higher adherence when generics are available. But here’s the catch: if they’re not educated, cost becomes a red flag. “If it’s so cheap, is it safe?” That’s the unspoken question. And it’s not irrational. In countries with weak regulation, bad generics have caused real harm. In the U.S. and EU, that’s rare. But perception doesn’t care about statistics. It cares about stories.How Measurement Tools Are Changing
Researchers are no longer just asking patients, “Are you satisfied?” New tools use machine learning to scan social media, pharmacy records, and even voice tone in phone calls. One 2024 study analyzed 500,000 posts across 28 languages and found that patients in collectivist cultures (like Japan or Brazil) were 32% more likely to report satisfaction with generics than those in individualist cultures (like the U.S. or Germany). Why? In collectivist cultures, trusting authority (doctor, pharmacist, government) is built in. In individualist cultures, patients want to make their own decisions-and distrust anything they didn’t choose. The FDA’s new GDUFA III initiative is funding tools that track real-world outcomes: hospital visits, lab results, refill patterns. If a patient switches to a generic and their blood pressure stays stable? That’s proof. Not opinion.What Works: Simple Fixes for Better Acceptance
You don’t need fancy tech to improve patient satisfaction with generics. Just three things:- Explain the switch. Don’t assume they know what “bioequivalent” means. Say: “This is the same medicine, made by a different company. It’s cheaper, but just as safe.”
- Keep packaging consistent. If possible, use generics with similar shape, color, or imprint to the brand. Familiarity reduces anxiety.
- Follow up. Call or message patients a week after switching. Ask: “How are you feeling?” Not “Are you taking your meds?” That’s a conversation, not an audit.
The Bigger Picture
Generics save the U.S. healthcare system $300 billion a year. That’s money that could pay for cancer treatments, mental health services, or preventive care. But if patients stop taking them because they think they don’t work, those savings vanish. Non-adherence kills. It’s not just a cost problem-it’s a human one. The solution isn’t to make generics cheaper. It’s to make them feel trustworthy. Brand psychology isn’t about logos or ads. It’s about the quiet, persistent belief that something is safe, reliable, and worth trusting. Generics don’t need a better marketing campaign. They need better conversations.What Patients Are Really Saying
One woman on HealthUnlocked wrote: “I switched from Prinivil to lisinopril. It worked the same. I saved $36 a month. I wish I’d done it sooner.” Another wrote: “I switched my antidepressant. I felt like I was losing my mind. I went back to the brand. My doctor said it was all in my head. Maybe it was. But my head needed to believe it.” The truth? Both are right. Generics work. But belief matters just as much as biology.Are generic medications really as effective as brand-name drugs?
Yes, by law, generic medications must contain the same active ingredients, dosage, strength, and route of administration as their brand-name equivalents. They’re tested for bioequivalence-meaning they’re absorbed by the body at nearly the same rate and extent. The FDA and EMA require generics to fall within an 80-125% confidence range of the brand. Studies show no clinical difference in outcomes for the vast majority of drugs. The differences patients report are usually psychological, not pharmacological.
Why do some patients feel generics don’t work as well?
It’s often due to brand psychology. Patients associate the look, color, or shape of a brand-name pill with how they feel. When that changes-even if the drug inside is identical-the brain interprets the difference as reduced effectiveness. This is especially common with medications for chronic conditions like thyroid disease, epilepsy, or depression, where small changes in absorption can feel significant. Stress, anxiety about switching, and past negative experiences also amplify these perceptions.
Which types of medications have the lowest patient satisfaction with generics?
Antiepileptics, thyroid medications (like levothyroxine), and antidepressants have the lowest satisfaction rates with generics. These are drugs with narrow therapeutic windows-small changes in blood levels can cause noticeable side effects or reduced effectiveness. Patients on these medications are often highly sensitive to even minor variations, and many have had long-term success with a specific brand, making them reluctant to switch. Studies show satisfaction drops to around 69% for antiepileptics, compared to 85% for antibiotics.
Can healthcare providers improve patient satisfaction with generics?
Absolutely. When doctors and pharmacists explain why generics are safe and equivalent-using clear, non-technical language-patient satisfaction increases by up to 41%. Simply saying “it’s the same” isn’t enough. Patients need context: “This is the same medicine, just made by a different company under strict government rules.” Showing FDA or EMA approval documents, explaining bioequivalence standards, and checking in after the switch makes a big difference.
Do generic medications have different side effects?
The active ingredient causes the side effects, and that’s identical in generics. But inactive ingredients (fillers, dyes, coatings) can vary. For most people, this doesn’t matter. But for those with rare allergies or sensitivities (like lactose intolerance or dye allergies), a different filler might cause discomfort. That’s why some patients report new side effects after switching-not because the drug changed, but because something else in the pill did. Always tell your pharmacist about known allergies or intolerances.
How do cultural differences affect satisfaction with generics?
Yes, significantly. In collectivist cultures-like Japan, Brazil, or Saudi Arabia-patients are more likely to trust authority figures (doctors, pharmacists, regulators) and accept generics without question. In individualist cultures-like the U.S., Germany, or the UK-patients are more skeptical and want to make their own choices. Studies show satisfaction scores are 32% higher in collectivist cultures. This isn’t about intelligence or education; it’s about deeply held cultural norms around trust and decision-making.
Is there a way to measure patient satisfaction accurately?
Yes. The Generic Drug Satisfaction Questionnaire (GDSQ) is a validated 12-item tool that measures effectiveness, convenience, and side effects. More advanced methods include discrete choice experiments (DCE), where patients choose between hypothetical drug options, and machine learning models that analyze real-world data like refill rates and hospital visits. These tools help separate perception from reality. For example, a patient might say a generic “doesn’t work,” but if their blood pressure readings stay stable, the data says otherwise.
Why do generics cost so much less if they’re the same?
Brand-name drugs include the cost of research, clinical trials, marketing, and patent protection-often over $2 billion to bring one drug to market. Generics skip all that. They enter the market after the patent expires, using the existing safety and efficacy data. Their cost savings come from not repeating expensive steps. They’re not cheaper because they’re lower quality-they’re cheaper because they don’t carry the same overhead.