Shingles isn’t just a rash. It’s a burning, stabbing, electric pain that can last for weeks-or even years-if not handled right. If you’ve felt that sharp, localized sting on one side of your body, maybe along your ribs or forehead, you already know: this isn’t a simple skin issue. It’s your own virus, hiding in your nerves since childhood chickenpox, waking up and screaming for attention. And the clock is ticking.
Why Timing Matters More Than Anything
Antiviral drugs don’t cure shingles. They don’t erase the virus. But they can stop it from taking over your body-if you start them within 72 hours of the first sign of rash. That’s it. Three days. After that, the virus has already damaged your nerves, and the drugs lose most of their punch.
Studies show that starting antivirals early cuts the worst pain by about 30% and heals blisters two to three days faster. One patient in Bristol, 67, waited five days to see her GP. By the time she got valacyclovir, the blisters had turned into open sores. She ended up with post-herpetic neuralgia (PHN) for nine months. Another patient, 58, started acyclovir on day two. Her rash cleared in 10 days. No lingering pain.
The three main antivirals used are acyclovir, famciclovir, and valacyclovir. All work. But here’s what most doctors don’t tell you: valacyclovir is easier. You take it three times a day. Acyclovir? Five times. That’s a pill every four hours, including at night. Many people skip doses. Valacyclovir sticks better. It’s also more concentrated, so your body absorbs it better. For most adults, the standard dose is 1,000 mg three times daily for seven days.
What Happens If You Wait Too Long?
Waiting beyond 72 hours doesn’t mean treatment is useless. But the benefits shrink fast. By day 5, you’re mostly managing damage, not stopping it. The virus has already triggered inflammation in your nerves. That’s when the real pain begins-not from the rash, but from the nerves firing wrong signals. That’s post-herpetic neuralgia, or PHN. One in ten shingles patients gets it. For those over 60? One in three.
PHN isn’t just discomfort. It’s constant burning, itching, or shooting pain that can make sleeping, dressing, or even brushing your hair unbearable. And it doesn’t go away on its own. The longer you wait to treat shingles, the higher your risk. That’s why the CDC and Mayo Clinic both say: if you suspect shingles, don’t wait. Call your doctor today.
Can Antivirals Prevent Chronic Pain?
This is where things get messy. Some studies say yes. Others say no. The Cochrane Review says acyclovir doesn’t reduce PHN at six months. But a 2011 meta-analysis found early antivirals cut PHN risk by 20-30%. So which is right?
The answer might be in the details. People who start treatment within 48 hours-not just 72-have the best outcomes. And valacyclovir seems to do better than acyclovir at reducing nerve pain, even if both clear the rash at the same speed. A 2023 study from NYU tracked patients with eye shingles (HZO). Those on long-term low-dose valacyclovir (500 mg daily) used 25% less gabapentin and had fewer flare-ups. That’s huge. Eye shingles can cause blindness. Reducing pain meds and flare-ups? That’s life-changing.
Still, don’t expect miracles. About 38% of patients who took antivirals on time still got PHN, according to PatientsLikeMe. That’s why pain management isn’t optional-it’s essential.
Pain Management: Beyond the Pills
Shingles pain isn’t like a headache. It’s neuropathic. That means regular painkillers like ibuprofen or paracetamol won’t touch it. You need drugs that calm overactive nerves.
- Gabapentin or pregabalin: These are anti-seizure drugs that calm nerve signals. Start low-300 mg once a day. Increase slowly. Side effects? Dizziness, drowsiness. Older adults are especially sensitive.
- Amitriptyline: A cheap, old-school antidepressant that helps nerves stop screaming. Take 25-75 mg at night. It helps sleep too. But it can dry your mouth, make you constipated, or cause dizziness.
- Lidocaine patches: These stick right on the painful area. Wear for 12 hours, take off for 12. No systemic side effects. Great for localized pain.
- Capsaicin cream: Made from chili peppers. It burns at first-then numbs. Use 0.075% cream, 3-4 times a day. Wash hands after. Don’t touch your eyes.
For severe pain, doctors might prescribe short-term opioids. But they’re risky. Opioids don’t work well for nerve pain, and addiction is real. Use them only if nothing else helps-and only for a few days.
The Eye Factor: Don’t Ignore It
If your shingles rash is near your eye-forehead, nose, eyelid-this is an emergency. Ophthalmic shingles (HZO) can cause scarring, glaucoma, or permanent vision loss. The Zoster Eye Disease Study showed that long-term, low-dose valacyclovir (500 mg daily) reduced new eye problems by 26% and flare-ups by 30% over 18 months.
Most doctors don’t think to prescribe this. But if you have eye involvement, ask about extended antiviral therapy. The American Academy of Dermatology now recommends it for high-risk cases. Don’t wait until your vision blurs. Act early.
What About Steroids?
Some doctors add prednisone-a steroid-to antivirals. The idea: reduce inflammation faster. A few small studies show better pain control in the first week. But steroids weaken your immune system. That’s dangerous if you’re older, diabetic, or have other conditions. The Mayo Clinic says the evidence isn’t strong enough to recommend it routinely. It’s a gamble. Only consider it if your pain is extreme and you’re otherwise healthy.
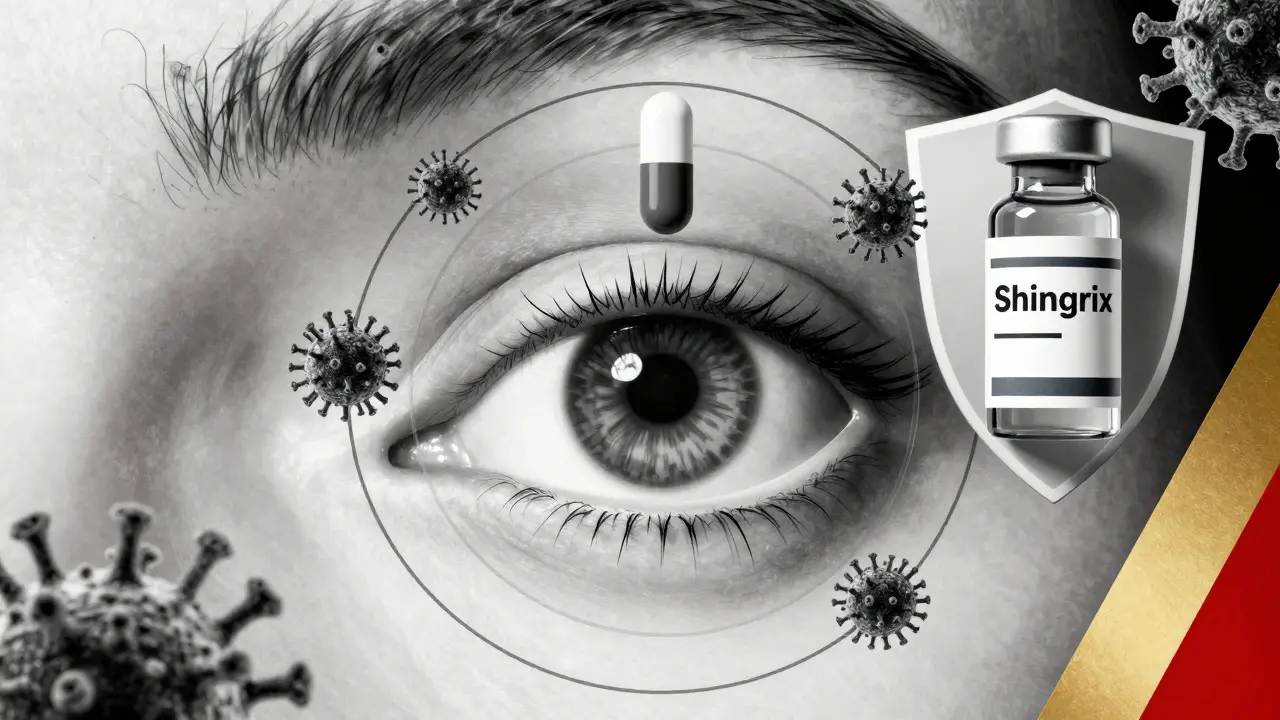
The Vaccine: Your Best Defense
Shingrix is the only shingles vaccine recommended in the UK and US. It’s 90% effective at preventing shingles. Even if you get it after vaccination, the rash is milder and the chance of PHN drops by 90%. Two doses, 2-6 months apart. You need it even if you had shingles before. Or if you had the old vaccine (Zostavax). That one doesn’t work anymore.
It’s for adults 50+ and anyone 19+ with a weakened immune system. Side effects? Sore arm, fatigue, headache. Worth it. The cost? Around £150-£200 for both doses privately. But in the UK, it’s free on the NHS for people aged 70-79. Check your eligibility.
What to Do Right Now
If you think you have shingles:
- Look for pain, tingling, or burning on one side of your body-before the rash appears.
- Check for red patches turning into fluid-filled blisters in a band.
- Call your GP today. Don’t wait until tomorrow.
- Ask for valacyclovir 1,000 mg three times daily for 7 days.
- If the rash is near your eye, ask for an urgent eye exam.
- Start gabapentin or amitriptyline if pain is severe.
- Use lidocaine patches or capsaicin cream for local relief.
Shingles is not something you ride out. It’s a medical event. The faster you act, the less pain you’ll carry for months-or years.
What’s Next?
Research is moving fast. Scientists are now looking at genetic markers that predict who’s more likely to get PHN. Some are testing nerve-blocking injections for early-stage pain. Others are studying whether combining antivirals with anti-inflammatory herbs like curcumin helps. But right now, the best tools are still antivirals and nerve-targeted pain meds.
If you’ve had shingles and are still in pain, don’t give up. PHN can improve-even years later-with the right combination of meds, physical therapy, and nerve stimulation devices. You’re not alone. And it’s not your fault.
Can shingles be cured with antivirals?
No. Antivirals don’t cure shingles or kill the virus hiding in your nerves. They slow down the active outbreak, reduce pain, and help the rash heal faster-but the virus stays dormant. That’s why shingles can come back, though it’s rare.
How soon should I start antivirals for shingles?
Within 72 hours of the rash appearing. The sooner, the better. Starting within 48 hours gives you the best chance to reduce pain and prevent complications like post-herpetic neuralgia. Waiting beyond three days greatly reduces the benefit.
Is valacyclovir better than acyclovir for shingles?
Valacyclovir is easier to take-three times a day versus five for acyclovir-and may reduce nerve pain slightly better. Both clear the rash equally fast. For most people, valacyclovir is preferred because adherence is higher, and side effects are similar.
Can I get shingles from someone else?
No. You can’t catch shingles from someone else. But if you’ve never had chickenpox or the vaccine, you can catch chickenpox from their shingles rash-through direct contact with the fluid. Once you’ve had chickenpox, the virus stays in your body and can reactivate as shingles later.
Does the shingles vaccine prevent post-herpetic neuralgia?
Yes. The Shingrix vaccine reduces the risk of post-herpetic neuralgia by about 90%. Even if you get shingles after vaccination, the pain is usually much milder and shorter. It’s the best protection against long-term nerve damage.
Why does shingles hurt so much?
The varicella-zoster virus attacks your sensory nerves. When it reactivates, it causes inflammation and damage to nerve fibers. These damaged nerves send chaotic, exaggerated pain signals to your brain-even when there’s no injury. That’s why the pain feels like burning, stabbing, or electric shocks.
Can I use ibuprofen for shingles pain?
Ibuprofen or paracetamol might help with mild discomfort or fever, but they won’t touch the nerve pain. Shingles pain is neuropathic, meaning it comes from damaged nerves, not inflammation. You need medications like gabapentin or amitriptyline that target nerve signaling.
How long does shingles pain last?
The rash usually clears in 2-4 weeks. But nerve pain can linger. For most people, it fades in 1-3 months. For 10-18% of patients-especially over 60-it lasts longer than three months. That’s called post-herpetic neuralgia. The earlier you treat the outbreak, the lower your risk.
Is shingles contagious?
Shingles itself isn’t contagious. But the virus in the blisters can spread to someone who’s never had chickenpox or the vaccine. They’d get chickenpox, not shingles. Cover the rash, avoid touching it, and wash your hands. Once the blisters scab over, you’re no longer contagious.
Should I stay home if I have shingles?
Yes, especially if your rash is oozing and not covered. Avoid close contact with pregnant women who haven’t had chickenpox, newborns, and anyone with a weak immune system. Once the blisters crust over, you can return to normal activities. Rest helps your body fight the virus.