Sulfonylurea Hypoglycemia Risk Calculator
This calculator estimates your risk of experiencing low blood sugar while taking sulfonylurea diabetes medications based on factors discussed in the article. Your results will help you discuss risk reduction strategies with your healthcare provider.
Why Sulfonylureas Can Cause Low Blood Sugar
Sulfonylureas are old-school diabetes pills that force your pancreas to release more insulin-no matter what your blood sugar is doing. That’s great for lowering high glucose, but it’s also why you can crash into hypoglycemia so easily. These drugs work by locking onto special receptors on your beta cells, tricking them into pumping out insulin even when your body doesn’t need it. The result? Blood sugar drops below 70 mg/dL, and suddenly you’re sweating, shaking, or confused-sometimes without warning.
It’s not just about taking the pill. It’s about what happens after. Unlike newer drugs that only act when glucose is high, sulfonylureas keep working for hours, even overnight. That’s why so many people on these meds wake up with nightmares: drenched in sweat, heart racing, unable to think straight. One Reddit user, Type2Warrior87, wrote in March 2023: “Switched from metformin to glyburide last month and have had 3 severe lows requiring glucagon-my doctor didn’t warn me this could happen multiple times per week.”
The Biggest Culprit: Glyburide
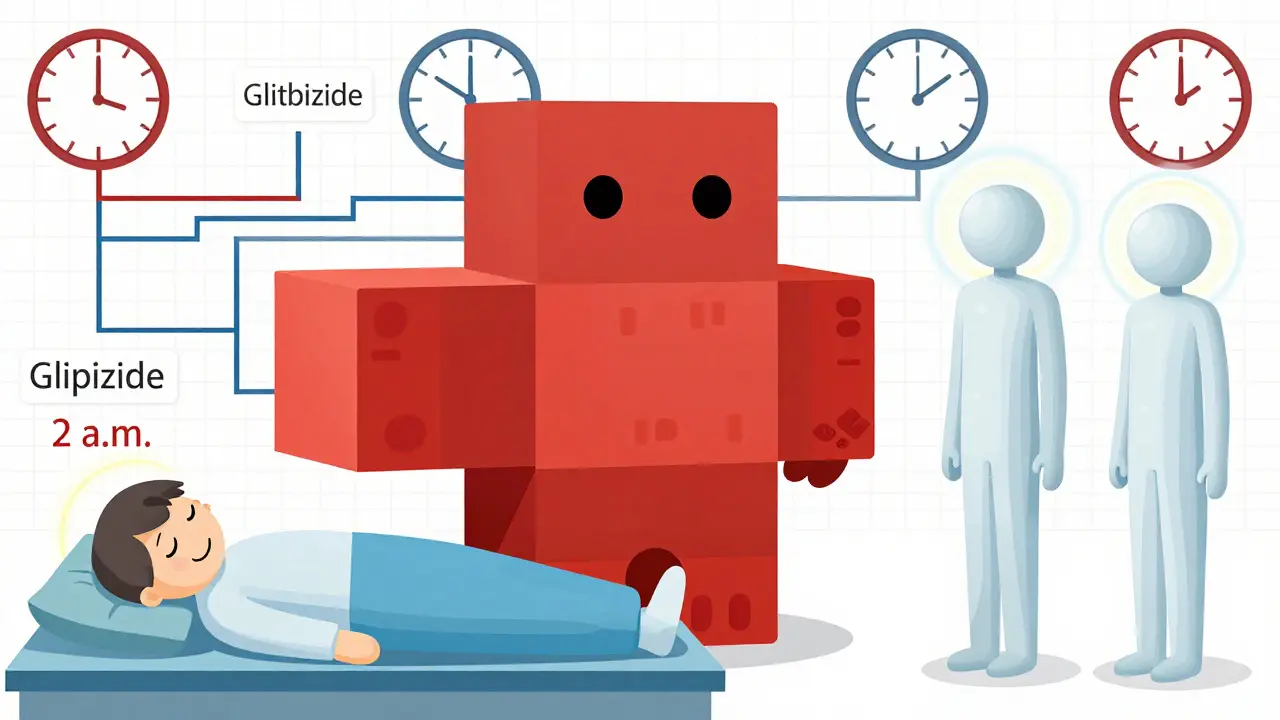
Not all sulfonylureas are the same. Glyburide (also called glibenclamide) is the most commonly prescribed in the U.S., making up about 70% of all sulfonylurea prescriptions. But it’s also the most dangerous when it comes to low blood sugar. Why? Because it sticks around. Its half-life is 10 hours, and it produces active metabolites that keep working even after the original dose wears off. That means a single morning pill can still be lowering your blood sugar at 2 a.m.
Studies show glyburide causes nearly 40% more severe hypoglycemia than glipizide or glimepiride. A 2017 study in Diabetes Care found hospitalizations for low blood sugar were 1.8 events per 100 person-years with glyburide-compared to just 1.2 with glipizide. The American Geriatrics Society’s Beers Criteria specifically says: avoid glyburide in people over 65. The risk is 2.5 times higher than with safer alternatives.
Which Sulfonylureas Are Safer?
If you’re on a sulfonylurea and worried about lows, ask your doctor about switching. Glipizide, glimepiride, and gliclazide are much better choices. Glipizide lasts only 2-4 hours and doesn’t build up toxic metabolites. Glimepiride has a longer action but is more targeted to pancreatic cells, reducing off-target effects. Gliclazide-widely used in Europe and Australia-is the safest of all, with a 28% lower risk of hypoglycemia than glyburide, according to a 2019 meta-analysis.
Here’s how they stack up:
| Drug | Half-Life | Severe Hypoglycemia Risk | Best For |
|---|---|---|---|
| Glyburide | 10 hours | High (1.8 events/100 person-years) | Avoid in elderly, high-risk patients |
| Glipizide | 2-4 hours | Low (1.2 events/100 person-years) | Patients with irregular meals |
| Glimepiride | 5-8 hours | Moderate | Once-daily dosing, stable routines |
| Gliclazide | 10-12 hours | Lowest among sulfonylureas | Long-term use, European patients |
One user, GlipizideSurvivor, shared on DiabetesDaily.com: “After switching from glyburide to glipizide, my hypoglycemia episodes dropped from weekly to once every 2-3 months.” That’s not luck-it’s pharmacology.
Who’s Most at Risk?
Age isn’t the only factor. Older adults are more vulnerable-not just because of slower metabolism, but because their bodies don’t fight back as well. When blood sugar drops, healthy people release epinephrine and glucagon to raise it. But in many older patients, that system weakens. Still, a 1998 JAMA study by MR Burge found that healthy elderly people on sulfonylureas often still had strong counterregulatory responses. So it’s not age alone-it’s frailty, kidney function, and other meds.
Genetics matter too. About 1 in 5 people carry a CYP2C9 gene variant (*2 or *3) that slows how fast their body breaks down sulfonylureas. This can double or even triple hypoglycemia risk. If you’ve had repeated lows despite low doses, ask about genetic testing. The PharmGKB now recommends genotyping before starting sulfonylureas, especially if you’re on glyburide.
Drugs That Make Hypoglycemia Worse
Many common medications can turn a safe sulfonylurea dose into a dangerous one. Sulfonamide antibiotics, gemfibrozil (for cholesterol), and warfarin can all push sulfonylureas off protein-binding sites, freeing up more active drug into your bloodstream. Gemfibrozil alone can increase glyburide exposure by 35% and raise hypoglycemia risk by over two-fold.
If you’re on a sulfonylurea and your doctor adds a new pill-even something as simple as a cholesterol drug-ask: “Could this make my blood sugar drop too low?” A 2020 Drug Safety study showed that 1 in 6 sulfonylurea users had a dangerous interaction they weren’t warned about.

How to Prevent Low Blood Sugar
Prevention isn’t just about avoiding sugar. It’s about structure.
- Start low, go slow. The ADA recommends beginning with glyburide at 1.25 mg or glipizide at 2.5 mg. Most people don’t need more. Titrate only after 1-2 weeks.
- Eat on time. Skipping meals is the #1 trigger. Even one missed lunch can send you into a crash if you’re on glyburide.
- Carry fast-acting carbs. Always have 15g of glucose-glucose tabs, juice, or candy-within reach. Don’t wait until you’re shaking.
- Use a CGM. The DIAMOND trial showed continuous glucose monitors cut hypoglycemia time by 48% in sulfonylurea users. You don’t need to guess when your sugar’s dropping.
- Know your symptoms. Sweating (85% of cases), shakiness (78%), irritability (65%), confusion (52%)-these aren’t “just stress.” They’re your body screaming for sugar.
Structured education cuts hypoglycemia rates by 32%. If your clinic doesn’t offer a diabetes self-management class, ask for one.
When Sulfonylureas Still Make Sense
Yes, newer drugs like SGLT-2 inhibitors and GLP-1 agonists have far lower hypoglycemia risk-less than 0.3 events per 100 person-years. But they cost $500-$1,000 a month. Generic glipizide? About $4.00. That’s not a typo.
For people on fixed incomes, without insurance, or in countries with limited access to newer meds, sulfonylureas are still life-saving. The ADA and EASD agree: they’re appropriate when used carefully. A 2021 analysis showed they save $1,200-$1,800 per patient annually compared to newer agents-with no loss in HbA1c control.
The key isn’t avoiding sulfonylureas entirely. It’s using the right one, at the right dose, in the right person.
The Future: Genes, Monitoring, and Smarter Dosing
The next big shift isn’t about ditching sulfonylureas-it’s about personalizing them. The RIGHT-2.0 trial, wrapping up in late 2024, is testing a dosing system based on CYP2C9 genetics. Early results show it could slash hypoglycemia by 40%.
Another promising path: combining low-dose sulfonylureas with GLP-1 agonists. The DUAL VII trial found this combo reduced hypoglycemia by 58% compared to sulfonylurea alone. You get the cost savings of the old drug, with the safety of the new.
For now, if you’re on a sulfonylurea and have had even one low blood sugar episode, talk to your doctor. Ask: Is this the right drug? Is my dose too high? Should I switch? Should I get a CGM?
Low blood sugar isn’t just inconvenient. It’s dangerous. It’s linked to higher heart attack risk and death. But it’s also preventable-with the right knowledge, the right drug, and the right plan.