Most prescriptions you get filled are generics. They’re cheaper, just as effective for most people, and used in 90% of all U.S. prescriptions. But sometimes, your doctor writes a prescription that says "do not substitute" or "brand medically necessary". If you’ve seen that on your script, you might wonder: Why not just give me the generic? The answer isn’t always about profit or preference-it’s often about safety, biology, and real-world outcomes.
When Generics Aren’t Enough
For most medications-like blood pressure pills, statins, or antibiotics-generics work just as well. The FDA requires them to deliver the same active ingredient, in the same amount, with the same effect. But there’s a group of drugs where even tiny differences matter. These are called narrow therapeutic index (NTI) drugs. That means the difference between a dose that works and one that causes harm is razor-thin. Examples include:- Levothyroxine (Synthroid, Tirosint) for thyroid conditions
- Warfarin (Coumadin) for blood thinning
- Levetiracetam (Keppra) for seizures
- Lithium for bipolar disorder
The American Thyroid Association and the American Academy of Neurology both recommend sticking with the same brand for these drugs. Why? Because even small changes in how the drug is absorbed can throw your levels off. One study found that 12.7% of epilepsy patients had breakthrough seizures after switching from brand Keppra to a generic. Only 4.3% had seizures while staying on the brand. That’s not a small risk.
For thyroid patients, switching generics can mean your TSH levels swing unpredictably. One patient on Reddit shared: "Switched from Synthroid to generic twice. Both times, I got severe depression and brain fog. Went back to Synthroid-symptoms vanished in two weeks." That’s not anecdotal fluff. It’s backed by data showing inconsistent absorption between generic manufacturers, especially with levothyroxine.
Why Doctors Still Write Brand-Only Prescriptions
You might think doctors do this because they’re paid to push brand drugs. But the real reasons are more nuanced-and often tied to experience, not profit.- Past patient reactions: If a patient had a bad reaction to a generic version-like nausea, dizziness, or a flare-up of symptoms-the doctor will avoid repeating it.
- Inactive ingredients: Generics use different fillers, dyes, or coatings. For some people, those cause allergies or stomach upset. One common complaint? Switching from brand to generic ciprofloxacin led to diarrhea or cramps because of a different binder.
- Delivery systems: Some drugs rely on special delivery methods. Advair’s Diskus inhaler, for example, has a precise powder-dosing mechanism. Generic versions may look similar, but if the mechanics differ slightly, the dose delivered can be off.
- Consistency over time: Generic manufacturers change. One batch might come from Company A, the next from Company B. Even if both are FDA-approved, the absorption rate can vary. For chronic conditions, that inconsistency adds risk.
According to the Institute for Safe Medication Practices, only three situations truly justify brand-only prescribing: NTI drugs, patient-specific reactions to inactive ingredients, or documented failure with multiple generics. Yet a 2020 study from Johns Hopkins found that only 3% of brand-name prescriptions meet those criteria. The rest? Often just habit, fear of change, or patient pressure.
The Cost Difference Is Staggering
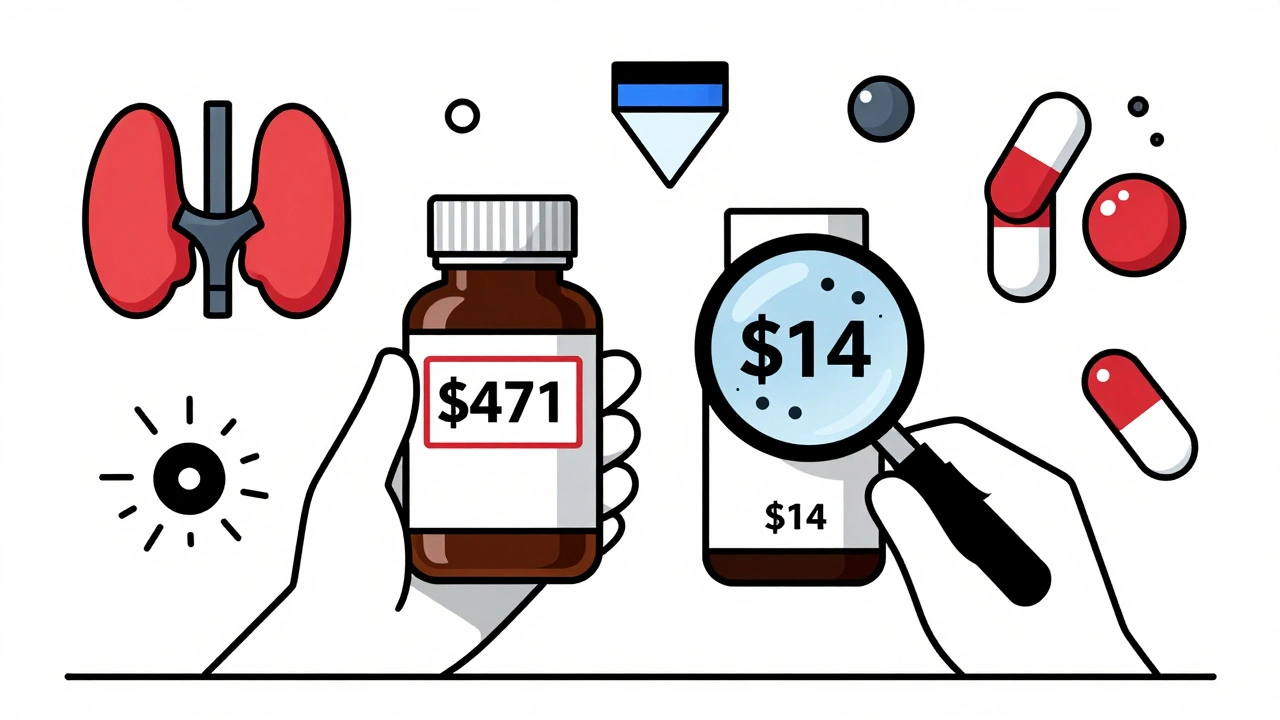
Let’s talk numbers. In 2022, the average brand-name prescription cost $471.67. The generic version? $13.76. That’s a 97% drop. For patients on high-deductible plans or without insurance, that gap can mean skipping doses, splitting pills, or going without.When a doctor prescribes brand-name when it’s not medically needed, patients pay more. A 2021 Kaiser Family Foundation survey found that 42% of patients with brand-only prescriptions paid significantly more out-of-pocket. One woman wrote: "My doctor prescribed brand-name lisinopril. I paid $180/month. Switched to generic-$4. I saved $1,700 a year. Why didn’t he suggest that?"
Generics make up just 23% of total U.S. drug spending. That means 77% of the money spent on prescriptions goes to brand-name drugs-even though generics handle 90% of the volume. That’s not because generics are worse. It’s because brand-name drugs are priced like luxury goods, not life-saving medicine.
What You Can Do
You’re not powerless when your doctor writes a brand-only script. Here’s what to ask:- "Is this medically necessary?" Don’t be afraid to push back. Say: "I’ve heard generics are fine for most drugs. Is there a specific reason we need the brand?"
- "Can we try the generic first?" If it’s not an NTI drug, ask for a trial. Monitor your symptoms. If nothing changes, stick with it.
- "Can you check the FDA’s Orange Book?" It lists which generics are rated as therapeutically equivalent. Your doctor might not know the latest ratings.
- "What’s the cost difference?" Sometimes, knowing the price makes the decision easier. Use GoodRx or your pharmacy app to compare.
Also, talk to your pharmacist. They see what works and what doesn’t. If you’ve had issues with a generic before, tell them. They can flag it in your record and alert the doctor.
Insurance and Paperwork
If your doctor writes "brand medically necessary," your insurance will likely require prior authorization. That means the insurer reviews the request before approving coverage. Processing time? Usually 72 hours. Approval rates vary:- Antiepileptics: 89% approved
- Thyroid meds: 82% approved
- Proton pump inhibitors (like omeprazole): Only 45% approved
Why the difference? Because insurers know most PPIs have excellent generic alternatives. They’re not going to pay $200 for a brand when $5 works just as well.
State rules also matter. In California, doctors must check a box labeled "Medical Necessity" on electronic prescriptions. In New York, they must write a detailed clinical reason. Texas has special rules for certain drugs. These rules exist to stop unnecessary brand prescribing.

The Bigger Picture
Pharmaceutical companies spend billions marketing brand-name drugs to doctors. Drug reps visit clinics, hand out samples, and promote brand familiarity. A 2018 study found that doctors who use brand names more often are more likely to prescribe them-even when generics are identical. It’s not malice. It’s psychological. We remember names we hear often.But the system is changing. The FDA now requires generic manufacturers to match brand drug shapes and sizes to reduce confusion. And "authorized generics"-made by the original brand company but sold under a generic label-are growing. They eliminate variability because they’re the exact same product, just cheaper.
Still, experts predict that by 2025, 15-20% of prescriptions will still be unnecessarily brand-only. That’s not because of science. It’s because of inertia, marketing, and lack of awareness.
Patients who ask questions, check prices, and push for generics aren’t being difficult. They’re saving money, reducing waste, and helping the system work better. You’re not just a patient. You’re a partner in your care.
When Brand-Name Is the Right Choice
Let’s be clear: brand-name drugs aren’t bad. Sometimes, they’re the only safe option. If you have epilepsy, a thyroid disorder, or take warfarin, staying on the same brand can prevent life-threatening complications. If you’ve tried a generic and had a bad reaction, your doctor is right to avoid it again.The issue isn’t brand vs. generic. It’s appropriate use. For 90% of medications, generic is the smart, safe, affordable choice. For the other 10%, brand-name is medically necessary. The goal isn’t to eliminate brand drugs-it’s to eliminate unnecessary ones.
If you’re unsure, ask. If you’re paying too much, speak up. And if your doctor says, "This one’s different," ask them to explain why-with evidence, not just tradition.
Can I ask my doctor to switch from a brand-name drug to a generic?
Yes, absolutely. You have the right to ask why a brand-name drug is being prescribed and whether a generic is an option. If it’s not a narrow therapeutic index drug, a generic is likely just as effective. Ask your doctor to explain the medical reason if they say no. Many times, they’ll agree to try the generic if you’ve had no issues with generics before.
Why do some generics make me feel worse?
Generics have the same active ingredient, but they can use different fillers, dyes, or coatings. For some people, those inactive ingredients cause side effects like stomach upset, headaches, or rashes. This is especially common with antibiotics like ciprofloxacin or thyroid meds like levothyroxine. If you notice a change after switching, tell your doctor and pharmacist. You may need to stick with the brand or try a different generic manufacturer.
Are all generics the same quality?
All FDA-approved generics must meet the same standards for safety and effectiveness as brand-name drugs. But because different companies make them, the inactive ingredients and how the drug is absorbed can vary slightly. For most drugs, that doesn’t matter. For narrow therapeutic index drugs, it can. That’s why consistency matters-stick with the same manufacturer if you’re doing well on it.
What does "do not substitute" mean on my prescription?
It means the pharmacist is legally required to give you the brand-name drug, even if a generic is available. This must be written clearly by your doctor. Without this note, the pharmacist can legally switch you to a generic. If you see this on your script and aren’t sure why, ask your doctor for the reason.
Can insurance deny coverage for a brand-name drug?
Yes. If your doctor prescribes a brand-name drug without a clear medical reason, your insurance may require prior authorization or deny coverage entirely. You’ll then have to pay out-of-pocket or switch to a generic. Some insurers approve brand-name drugs for NTI medications like levothyroxine or warfarin, but rarely for things like statins or blood pressure pills.