Have you ever filled a prescription and been shocked by the price-only to find out there’s no cheaper generic version available? It’s not a glitch. It’s not bad luck. It’s the system working exactly as designed-for drug companies, not patients. Some brand-name drugs sit on the market for decades without a single generic competitor, even after their patents expire. And the reasons why are more complicated than most people realize.
Patents Aren’t the Whole Story
Most people think once a drug’s patent runs out, generics automatically appear. That’s not true. A standard patent lasts 20 years from the date it’s filed, but that’s just the starting line. By the time a drug hits the market, years have already passed in clinical trials. So the real window for exclusive sales is often only 7 to 12 years. To stretch that, companies file multiple patents-not just on the active ingredient, but on the coating, the pill shape, the delivery method, even the way it’s packaged. Take Nexium, the acid reflux drug. Its original patent on esomeprazole expired in 2001. But AstraZeneca kept selling it at full price for another 13 years by filing new patents on a slightly different version. This tactic, called “product hopping,” isn’t illegal-it’s a standard part of the playbook. By the time a generic version finally came out in 2014, the company had already made billions.Complex Drugs Can’t Be Copied
Not all drugs are like aspirin. Some are made from biological materials that can’t be precisely replicated. Premarin, a hormone therapy made from pregnant mare’s urine, has been on the market since the 1940s. It contains a mix of 10 or more estrogen compounds, many of which aren’t even fully identified. No lab can recreate that exact blend. So even though its patents expired decades ago, there’s still no generic version. The same goes for biologics-drugs made from living cells, like Humira for rheumatoid arthritis or Enbrel for psoriasis. These aren’t simple chemicals. They’re complex proteins that behave differently depending on how they’re grown, purified, and stored. The FDA doesn’t call them “generics.” They’re called “biosimilars,” and getting approval takes 10 to 12 years of extra testing. Humira’s first biosimilar didn’t reach U.S. shelves until 2023-seven years after its patent expired.The FDA’s Tightrope Walk
The FDA requires generics to be “bioequivalent” to the brand-name drug. That means they must deliver the same amount of active ingredient into the bloodstream at the same rate. For most pills, that’s easy to prove. But for drugs with narrow therapeutic windows-like seizure meds, blood thinners, or thyroid pills-even a 5% difference can cause serious side effects or make the drug useless. That’s why the FDA demands extra testing for complex formulations. Inhalers like Advair Diskus? They need special studies to prove the generic version delivers the same dose to the lungs. Extended-release pills like Prozac Weekly? The timing of the drug release has to match exactly. These aren’t just paperwork hurdles-they require expensive equipment, specialized labs, and years of testing. Most generic manufacturers won’t bother unless they’re sure they can make a profit.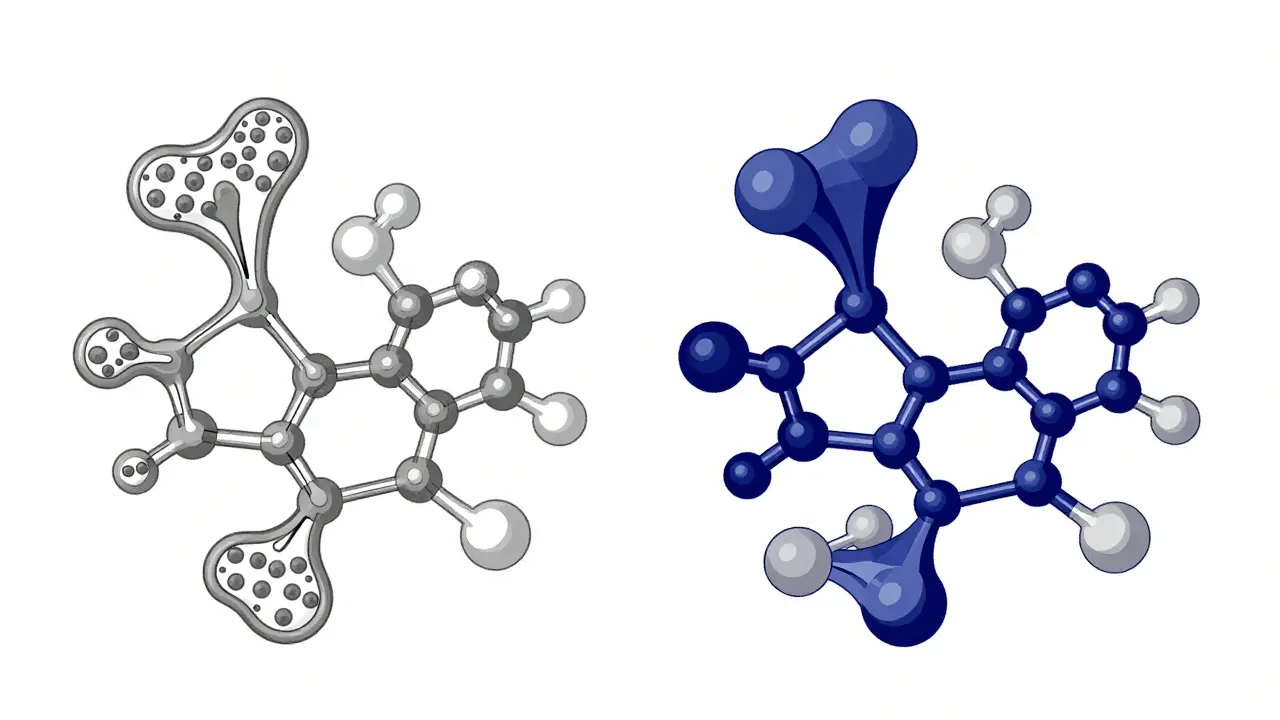
Patent Thickets and Pay-for-Delay
Big pharma doesn’t just rely on patents. They use them like a shield wall. A single drug can have 20, 30, even 50 patents listed in the FDA’s Orange Book. Many of these are minor tweaks-new salt forms, new packaging, new dosing schedules. These aren’t innovations. They’re legal tricks to block generics. Even worse is “pay-for-delay.” This is when the brand-name company pays a generic manufacturer to stay out of the market. The FTC found 297 of these deals between 1999 and 2012. One famous case involved the antibiotic azithromycin. The brand-name maker paid a generic company $100 million to delay launching its version for three years. That’s $100 million to keep prices high. And it’s legal-until recently. The CREATES Act of 2019 tried to shut this down by forcing brand-name companies to provide samples of their drugs to generic makers. Before that, some companies refused to sell samples, making it impossible for generics to test their versions. Now, they can be sued if they do.Why Some Drugs Stay Expensive Forever
Look at the EpiPen. Mylan raised the price from $100 to over $600 in a decade. Why? Because they kept changing the design-new needle, new casing, new packaging. Each tweak reset the clock on patent protection. Even when generics were approved, most patients didn’t switch. Doctors were used to prescribing EpiPen. Pharmacies stocked it. Insurance plans favored it. And patients were scared to try something new for something that could save their life. Oncology drugs are another big category. About 68% of cancer medications have no generic alternatives. Why? Because they’re made with intricate chemical processes. They require cold chains, sterile environments, and precision dosing. Making a generic version isn’t just hard-it’s risky. One mistake, and a patient gets the wrong dose. That’s why most generic companies avoid them.
The Real Cost of No Generics
The price difference isn’t just a number. It’s life or death for people on fixed incomes. A patient with chronic myeloid leukemia paid $14,500 a month for Gleevec before its patent expired in 2016. After generics came out, the cost dropped to $850. That’s a 94% drop. For many, that meant keeping the drug. For others, it meant choosing between rent and medicine. Medicare data shows that 22% of people taking drugs with no generic alternatives spend over $5,000 a year out of pocket. For those with generics, it’s only 8%. And it’s not just about money. One patient on PatientsLikeMe said the generic version of Spiriva didn’t work as well for her asthma-even though it had the same active ingredient. She felt it didn’t open her lungs the same way. That’s not placebo. That’s real variability in delivery systems.What’s Changing-and What’s Not
The FDA has started moving faster. In 2022, they approved 27% more complex generics than the year before. Biosimilars are on the rise too-32 were approved in 2022, and that number is expected to hit 75 by 2025. Insulin, long held hostage by patent battles, now has several biosimilars on the market. But progress is slow. Some drugs will never have true generics. Ultra-complex biologics. Drugs for rare diseases with tiny markets. Medicines made from biological sources that can’t be standardized. Experts estimate that by 2030, about 5% of all prescription drugs will still have no generic alternative. And those will stay expensive.What You Can Do
If your drug has no generic, ask your doctor: Is there another drug in the same class that does? For example, if you’re on Viibryd (vilazodone), a generic antidepressant like sertraline might work just as well. Pharmacists can help you find alternatives. Check the FDA’s Orange Book. It lists every patent and exclusivity period for brand-name drugs. You can see when a generic might arrive. And if you’re paying thousands a year for a drug with no cheaper option, speak up. Patient advocacy groups are pushing for reform. The system isn’t broken-it was built this way. But it doesn’t have to stay that way.Why can’t generics be made for all brand-name drugs?
Generics can’t be made for some drugs because they’re too complex to replicate exactly. Biologics, like Humira, are made from living cells and can’t be copied like a chemical pill. Others, like Premarin, use natural materials that can’t be standardized. Even for simpler drugs, the FDA requires strict testing to prove the generic works the same way-something that’s expensive and time-consuming for manufacturers.
Do generics work as well as brand-name drugs?
For most drugs, yes. The FDA requires generics to be bioequivalent-meaning they deliver the same amount of active ingredient into your bloodstream at the same rate. But for drugs with narrow therapeutic windows-like epilepsy meds, blood thinners, or thyroid pills-even small differences can matter. Some patients report feeling different on generics, especially with inhalers or extended-release pills. That doesn’t mean the generic is ineffective, but it may feel different.
How long does it take for a generic to come out after a patent expires?
It varies. For simple pills, it can be weeks or months. For complex drugs, it can take years. Legal battles, patent thickets, and delays in FDA approval can push it out for 5-10 years. Some drugs, like Humira, didn’t see their first biosimilar until seven years after patent expiry. And in rare cases, generics never come at all.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of chemical drugs. Biosimilars are highly similar-but not identical-to biologic drugs, which are made from living cells. Because biologics are complex, biosimilars can’t be exact replicas. They must undergo more testing to prove they work the same way. The approval process for biosimilars takes longer and costs more than for traditional generics.
Can I switch from a brand-name drug to a generic without my doctor’s approval?
In many cases, yes-pharmacists can substitute a generic unless the doctor writes “dispense as written” on the prescription. But for drugs with narrow therapeutic windows, your doctor may prefer you stay on the brand. Always talk to your doctor or pharmacist before switching, especially if you’re on medication for epilepsy, heart conditions, or thyroid disorders.
Why do some drugs stay expensive even after generics are available?
Sometimes, the brand-name company still controls the market through marketing, insurance partnerships, or patient assistance programs. Doctors may keep prescribing the brand because they’re used to it. Patients may stick with it out of fear or habit. And in some cases, the generic isn’t priced much lower-especially if only one company makes it. Competition drives prices down, and without enough generic makers, prices stay high.
Are there any new laws helping generics get approved faster?
Yes. The CREATES Act of 2019 stops brand-name companies from blocking access to drug samples needed for testing. The FDA’s GDUFA III program also prioritizes reviews of complex generics. And biosimilar pathways are improving. But progress is slow. The biggest hurdle isn’t law-it’s money. Making a generic for a complex drug costs millions. If the market is small, companies won’t invest.